Nitric Oxide administration in MRI
exp date isn't null, but text field is
Objectives
Nitric oxide delivery systems cannot be taken into the MRI scanner room, this document explains the configuration required for scanning a patient receiving inhaled NO.
Scope
This document applies only to patients who are intubated & ventilated receiving inhaled Nitric Oxide (NO) in PICU or NICU in RHC. NO can only be delivered in the 1st floor MRI scanner
Audience
All NICU, PICU and anaesthetic staff within RHC Glasgow
Administration of nitric oxide within the MRI scanner will be an uncommon procedure but cases will occasionally arise. Experience with patients in the past is that the delivery systems are awkward and the ergonomics have been poor in terms or equipment arrangement at the entrance to the scanning room. Alterations have been made in order that we can now use standard administration equipment and configure this in a way that will closely resemble a routine anaesthetic administration in MRI
Planning of potential cases MUST involve the anaesthetic department. It is possible to set up the entire breathing system in with NO at the required concentration running through the breathing system prior to collecting the patient from PICU / NICU. This will allow an easy transfer at the scanning room door with a simple switch of the patient breathing system connection.
The Nitric Delivery system can sit in the control room next to the monitor.

The nitric delivery & monitoring tubing are connected into the circle system as we would do in theatre i.e. delivery attachment directly onto the inspiratory limb of the circle and the monitoring / sampling line further up the inspiratory limb. Different types of soda lime have different effects in reducing both NO and NO2 within the circle system, whilst most of these are minor we do not recommend using low flow anaesthesia. [1]

We have put the sampling line in-between 2 tube extensions in this example.


2 or 3 sets of tubing extensions are required (depending of the position of your patient in the scanner) – work out the maximum distance when setting up the kit prior to calibration of the NO delivery system.
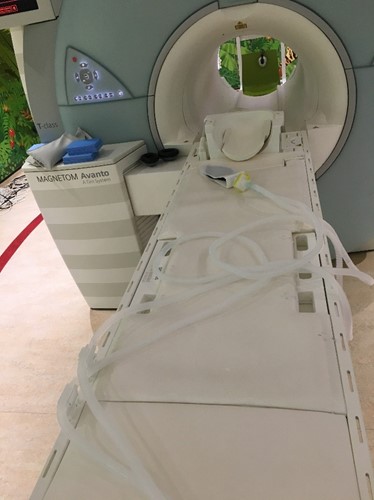
The gas tubes are long enough to move the anaesthetic machine all the way to sit on the left of the door at the internal side of the wave guides. Suction and scavenging have not been connected in this image – use the extension tubes hanging on the rear of the anaesthetic machine.


Once the system is assembled, put a test lung on the patient end, set up the ventilator to your patient’s requirements & run the calibration of the Nitric delivery system. You will need a flow of 10lpm of O2 through the circle system for this.
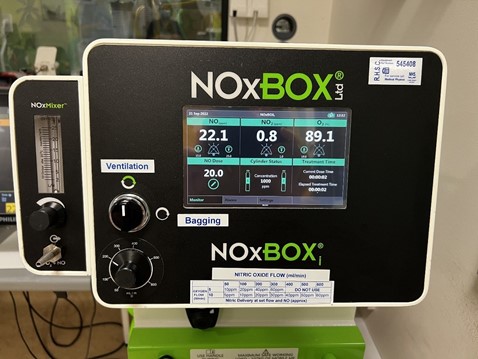
There is usually no need to set up a t-piece system for bagging. If the patient requires manual ventilation e.g. for ETT suction then this can be accomplished by switching to the bag on the circle system.
If a t-piece is required, it can be set up in advance & passed through the wave guide, but the user will be in scan and the selection of breathing system is in the control room, so it requires additional personnel & potentially awkward communication so it is recommended that the manual ventilation bag on the circle is used whenever possible.
MRI 1st Floor (main paediatric scanner) radiology Ex 84270 0141 452 4270
If you require further advice please contact Dr Graham Bell, graham.bell@ggc.scot.nhs.uk or mobile via switchboard
PICKETT, A.H. et al. The role of soda lime during administration of inhaled nitric oxide, British Journal of Anaesthesia, 72(6):683-685.
Last reviewed: 12 July 2023
Next review: 31 July 2026
Author(s): Dr Graham Bell, Consultant Anaesthetist; Dr Pauline Hall-Barrientos, Hospital Physics; Ms Marie Pirie, Superintendent Radiographer; Mr Kevin Jerome, Senior ODP
Approved By: Paediatric Guidelines Group
Document Id: 1095


