Heart murmurs in the neonate: an approach to the neonate with a heart murmur
exp date isn't null, but text field is
Audience
This guideline is applicable to medical and nursing staff caring for neonates in the West of Scotland.
- A heart murmur heard in the neonatal period may be associated with congenital heart disease.
- However, it must be remembered that not all infants with congenital heart disease have a heart murmur in the neonatal period.
- A neonate with any of the following findings needs urgent assessment including echocardiogram even if a murmur is not present: signs of heart failure or shock (see below), lower limb saturations <96% in the absence of respiratory disease, >3% difference between pre and post ductal saturations, absent/weak femoral pulses.
Investigation will vary depending upon local resources and expertise. The following recommendations represent the minimum requirements to ensure the safe management of neonates with heart murmurs and the timely identification of congenital heart disease.
- All infants with a heart murmur on neonatal examination should be reviewed by a senior paediatrician (middle grade or consultant).
- All infants with a heart murmur should remain in hospital until >24 hours old (unless definitive diagnosis is reached before this).
- All infant with a heart murmur should have a detailed cardiovascular clinical examination which must include measurement of pre and post ductal saturations.
- If a baby with a heart murmur is discharged before a definitive diagnosis is reached, the parents should be given a written information leaflet describing warning signs and advising them of what to do in the event that their baby became unwell.
Clinical examination:
- Dysmorphic features
- Signs of heart failure (tachypnoea, increased respiratory effort, hepatomegaly, shock)
- Palpation of brachial and femoral pulses
- Presence of cyanosis (as measured by lower limb saturations – a reading < 96% or >3% difference between pre and post ductal saturations should prompt further investigation 1)
- Heart sounds
- Presence of a heave
- Murmur – intensity, character, location and radiation
Electrocardiogram
- ECG has been shown to be a sensitive and specific tool for diagnosing atrioventicular septal defect2 (more common in infants with Trisomy 21) but has not been shown to aid significantly in the diagnosis of other structural congenital heart disease 3. It is not necessary to perform an ECG as part of the routine assessment of a baby with a heart murmur.
- If performed, a normal neonatal ECG shows right axis deviation because of the right ventricular dominance of the newborn heart. Left axis deviation in a newborn is a significant abnormal finding and should prompt further investigation.
- Whilst an abnormal ECG should prompt further investigation, a normal ECG should not be considered reassuring if there are abnormal clinical findings or lower limb saturations <96%.
CXR and 4 limb blood pressure
There is no evidence to support the use of CXR or 4 limb blood pressure measurements in the assessment of neonates with heart murmurs 3,4,5,6.
Echocardiography
- This is the gold standard investigation for differentiating between innocent and pathological murmurs. Some units will undertake an echocardiogram in all neonates with heart murmurs. For many units this is not currently practical.
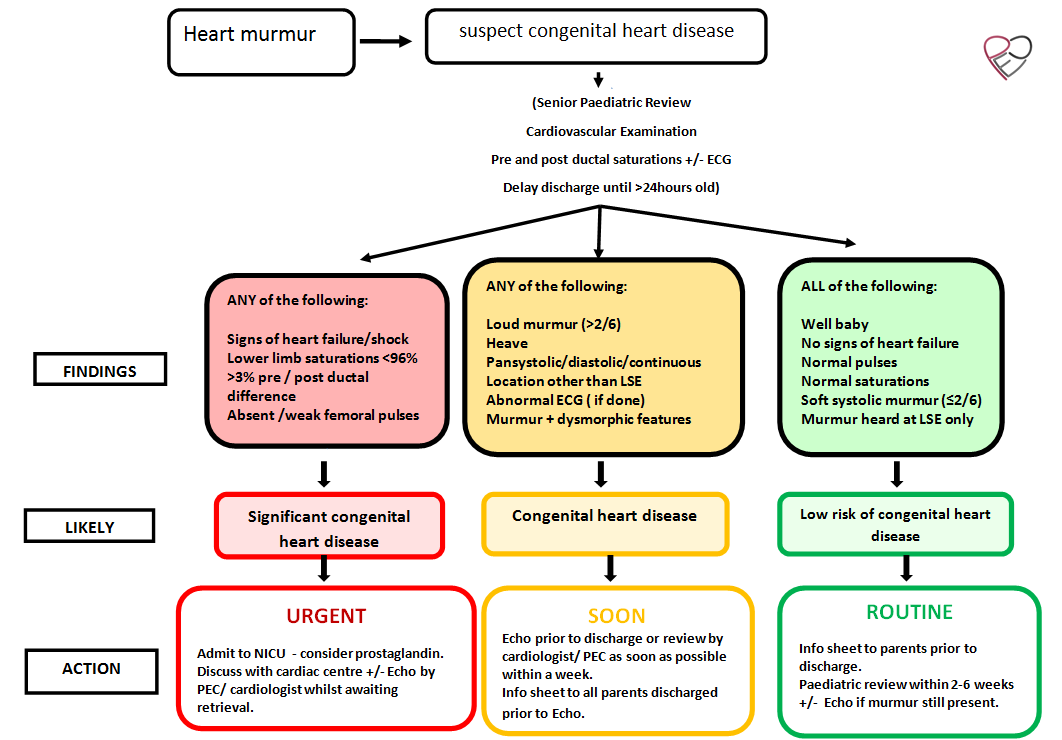
- In units where it is not feasible to perform echocardiogram for all infants with heart murmurs, information gathered from examination findings and oxygen saturations can be used to determine the need for and timing of echocardiography and follow up:
1. Likely significant congenital heart disease –urgent echocardiogram and review (same day)
Infants with a heart murmur and any of the following warning signs: lower limb saturations < 96%; >3% pre / post ductal difference; absent/weak femoral pulses; signs of heart failure or shock. These infants require admission to a neonatal unit for consideration of prostaglandin and urgent discussion +/- transfer to a cardiac centre. If appropriately skilled local PEC or visiting cardiologist is available to perform echocardiogram while retrieval is awaited then this can be linked by telemedicine link / used to update surgical centre. This should not be allowed to delay transfer.
2. Asymptomatic but clinically pathological murmur – soon echocardiogram (pre-discharge or as soon as possible within 1 week)
Infants without any of the above warning signs but with any of the following abnormal clinical findings: dysmorphism; heave; abnormal heart sounds; loud murmur (>2/6); pansystolic, diastolic, continuous murmur; murmur location other than left sternal edge/radiation.
3. Low risk of congenital heart disease - routine review neonatal OPC 2-6 weeks
Well infants with no signs of heart failure, normal pulses, lower limb saturations >96%, soft (1-2/6) systolic murmur at the left sternal edge with no radiation.
- Impact of pulse oximetry screening on the detection of duct dependent congenital heart disease: a Swedish prospective screening study in 39 821 newborns. Anne de Wahl Granelli et al BMJ 2009;338;a3037
- Neonatal ECG screening for congenital heart disease in Down syndrome. Narchi H Ann Trop Paediatr 1999; 19:51-4
- Can Cardiologists Distinguish Innocent from Pathologic Murmurs in Neonates? Andrew S Mackie et al The Journal of Pediatrics 2009;154:50-4
- Diagnostic value of chest radiography and electrocardiography in the evaluation of asymptomatic children with a cardiac murmur. Birkebaek NH, Hansen LK, Oxhoj H Acta Paediatr. 1995 Dec;84(12):1379-81
- Noninvasive tests in the initial evaluation of heart murmurs in children. Newburger JW, Rosenthal A, Williams RG, Fellows K, Mettinien OS. N Engl J Med. 1983 Jan 13;308(2);61-4
- Variability of four limb blood pressure in normal neonates. D S Crossland, J C Furness, M Abu-Harb, S N Sadagopan, C Wren Arch Dis Child Fetal Neonatal Ed 2004;89:F325-F327
Based on the PECSIG 2013 guideline
Last reviewed: 08 December 2021
Next review: 01 December 2024
Author(s): PECSIG Neonatal Murmur Guideline Group (Kathleen O’Reilly, Hilary Maddicks, Vishna Rasiah, Venu Gopalan with BCCA input from Rob Martin and John Simpson)
Co-Author(s): Adapted for local use by: Duncan Boyd, Maria Ilina, Brodie Knight and Kathleen O’Reilly.
Approved By: MCN for Neonatology West of Scotland

