Acute pain relief services protocol (APRS)
Objectives
To provide evidence based information and protocol based guidance for the provision of analgesia for paediatric patients.
Scope
Although this is intended to be used as an analgesic guideline for acute paediatric pain, it is not comprehensive and recommendations may not be appropriate for use in all circumstances.
Audience
This protocol is intended to be used by both nursing and medical professionals involved in the acute care of children during pre/post –op surgical management. It can also be used for range of acute pain management scenarios within other specialties, in the RHC, Glasgow.
Programming of major analgesic devices should only be undertaken by pain nurses, anaesthetists or appropriately trained staff. In addition, local anaesthetic top-ups should only be administered by anaesthetists.
Contact
For all pain enquires, APRS team are available Monday to Friday 0800-1600 on Ex 84319. Outwith these hours please contact the duty anaesthetist on call on Ex 84342 or Ex 84343.
Minimum monitoring standard for patients - MAJOR analgesic techniques (epidural, spinal, PCA/NCA/infusion)
- Patients should be centrally monitored when on wards
- Use of DECT phones is required.
- One nurse per 4 patients.
- Continuous pulse-oximetry.
- Hourly pain assessment and nurse recordings using the appropriate chart which are available in clinical areas.
- Regular visits by pain relief nurse specialist and/or duty anaesthetists
Minimum monitoring standard for patients ALL OTHER analgesic techniques
- Four hourly pain assessments should be carried out on the PEWS charts.
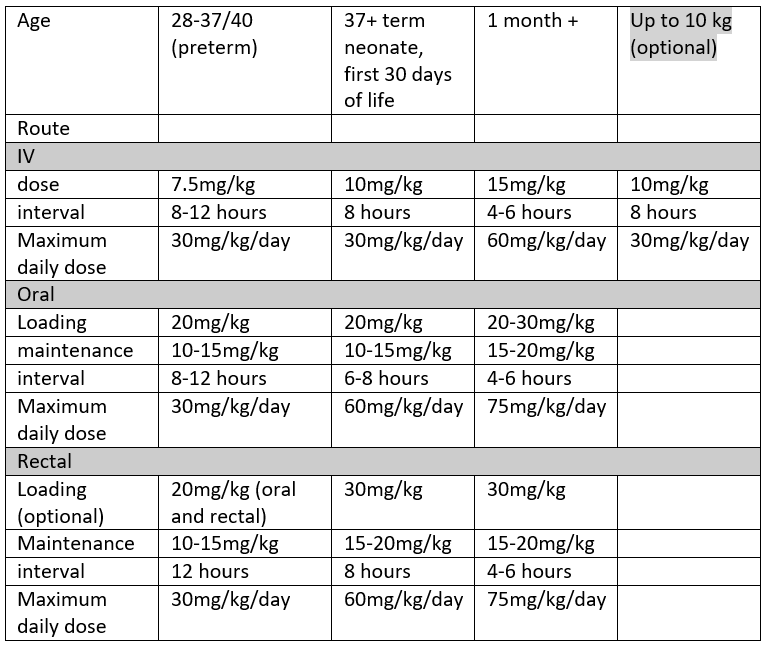
As per the WHO ladder, paracetamol is the first line non-opioid analgesic of choice in RHC. It can be given IV (usually only in theatre, in patients who are NBM or not tolerating oral diet, and in other specific circumstances), or Oral/Rectal. Dosing varies by age and by route chosen, as shown in the table below.
Guidelines can also be found in the BNFc by following this link BNF for Children
Disclaimer: For drug dosing in the context of infants in NICU, please refer to the Perinatal Network Monograph linked here: Local / Regional Drug Monographs - Scottish Perinatal Network
For some of the indications for use of paracetamol, BNFc uses age banded dosing. We would always advocate using weight based dose calculations wherever possible, as age banded dosing typically under doses at higher ages, and over doses at lower ages. This is particularly true for the extremes of weight within each age category.
Paracetamol dosing of 10mg/kg in under 10kg is a good rule of thumb for rotating trainees, and as a simple calculation can be used to minimise prescribing errors.
Obese children present a challenge when calculating their optimal therapeutic paracetamol dose. Literature on this is limited, but it is thought that paracetamol clearance is increased in obesity, which would mean a higher dose to achieve a therapeutic level. Most paediatric centres continue to use actual body weight to calculate paracetamol. An alternative is to use IBW (Ideal Body Weight). Calculating this requires height and is likely to lead to more prescribing errors. We recommend continuing to prescribe based on actual body weight, and within the maximum daily doses as above.
Caution should also be exercised in children with liver dysfunction and in neonatal unconjugated hyperbilirubinaemia. In these children we advise reducing the loading dose and increasing the dosing interval of paracetamol. In practical terms this would be 10mg/kg dosing, 8 hourly interval with a 30mg/kg/day limit, as for ‘term neonates’- see table above. Prescribing in children with haem oncological diagnoses should also be done with caution, and in consultation with the parent team. In these children, paracetamol may mask the fever which can accompany neutropenic sepsis.
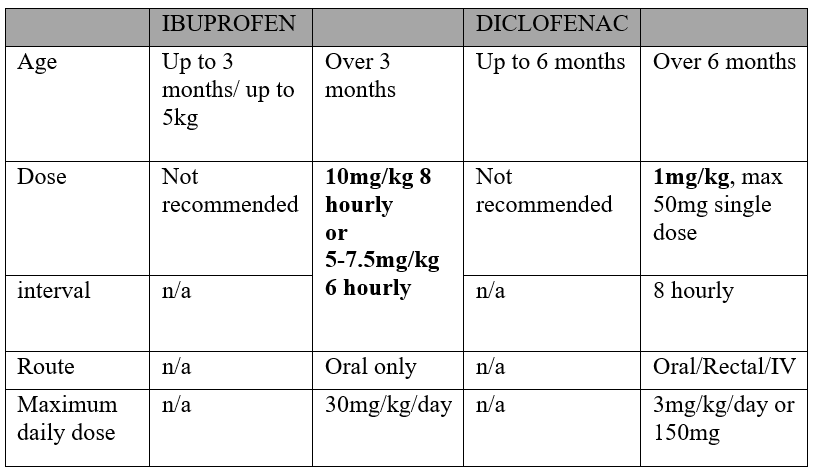
Non-Steroidal anti-inflammatory drugs such as diclofenac and ibuprofen are often prescribed in combination with paracetamol for post op pain relief, as well as for pain from a range of medical and surgical conditions.
Cautions/Contra-indications include:
- Bleeding risk.
- Severe Asthma.
- Renal dysfunction.
- GI ulceration/bleeding.
- On anticoagulants
NSAIDs should be used with caution in bone healing. In practical terms this would include fractures that have been or are likely to be difficult to unite, all distraction frames and most large bone grafts. In these cases, please discuss with the surgical team before prescribing regular NSAIDs.
As with paracetamol, cBNF predominantly uses age based dose banding for ibuprofen. We would again encourage calculating dose per kg.
Diclofenac is used less often, partly because it is more potent and thought to be more of a gastric irritant. It can be used for moderate to severe post op pain (for example it is used routinely for post op NUSS bar surgery) or pain from inflammation.
Dose guidance for NSAIDs can be found in the table below:
Disclaimer: For drug dosing in the context of infants in NICU, please refer to the Perinatal Network Monograph linked here: Local / Regional Drug Monographs - Scottish Perinatal Network
We recommend prescribing gastric protection alongside NSAIDS.
Omeprazole:
- Body weight 10-20kg: 10mg once daily PO
- Body weight >20kg: 20mg once daily PO
Morphine sulphate is the first line opioid used in RHC Glasgow.
However there may be occasions to use a different opioid, for example when there is an increase in morphine side effects or when switching opiates are appropriate.
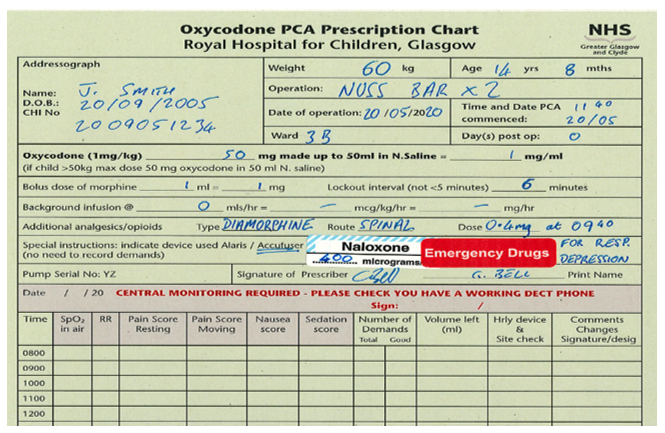
Oxycodone is the second line of opioid choice in RHC Glasgow.
Oxycodone is known to have a better side effect profile, with less itch, less nausea/vomiting, and less gastric stasis (ileus risk). It may therefore be chosen in preference to morphine in certain patients. Oxycodone is slightly more potent (between 1.5-2x) than morphine, but can be prescribed using the same dosing regimen as morphine, and titrated to effect.
Titration
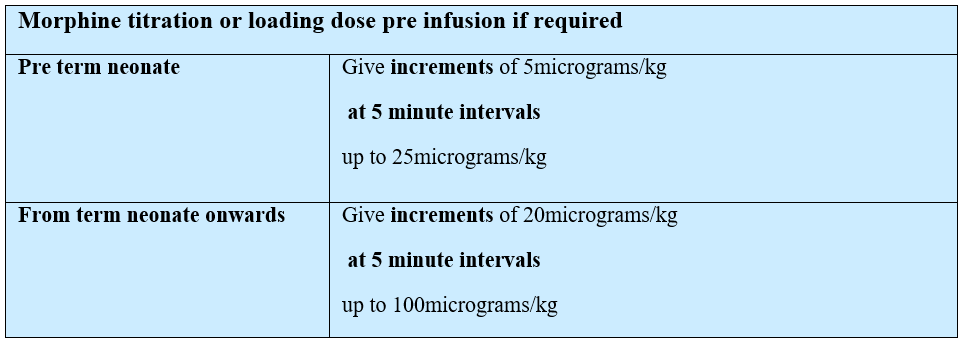
Intravenous morphine/oxycodone infusion
Dedicated anti-syphon/reflux infusion lines with maintenance fluids to ensure patency of cannula.
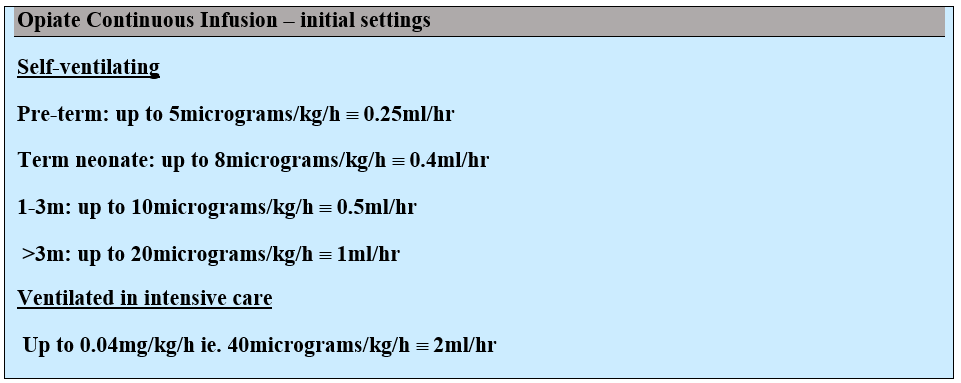
Morphine/Oxycodone syringe should be prepared as 1mg/kg in 50mls 0.9%saline º20micrograms/kg/ml; maximum 50mg in 50mls
Infusion only opiates are used almost exclusively in PICU and NICU. The settings below can also be used as a guide to initial background infusions for PCA/NCAs
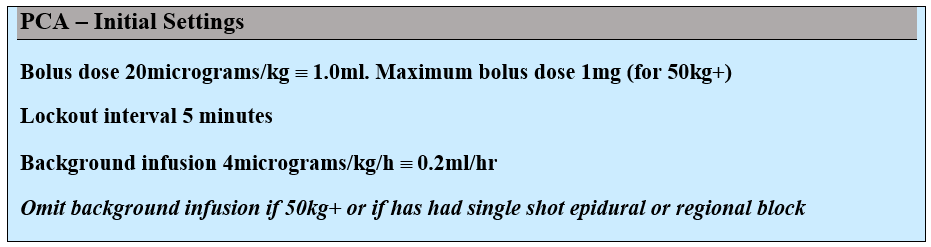
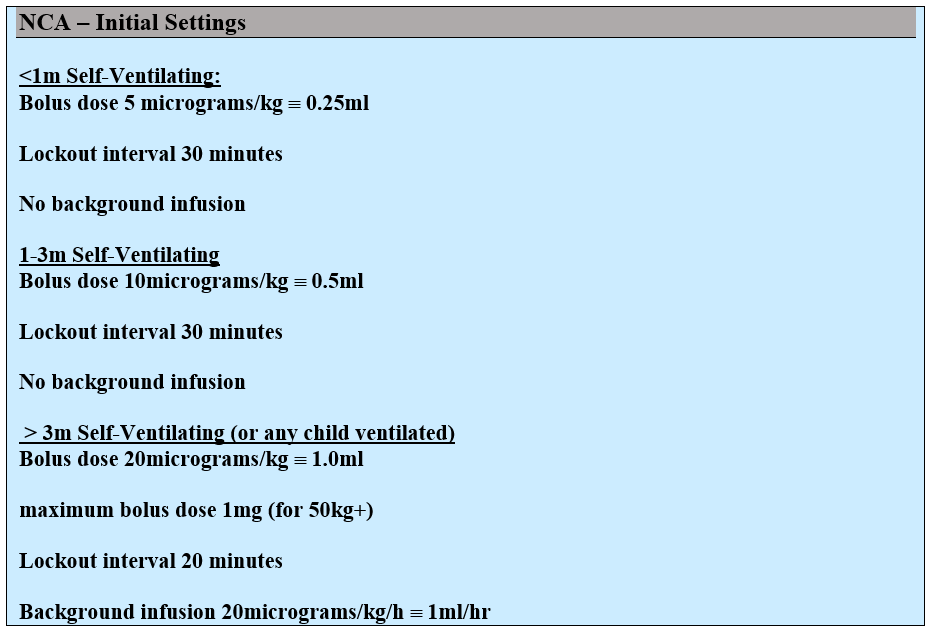
Morphine / oxycodone PCA or NCA
PCA (patient controlled analgesia) work well for children around 8 years and over, who can understand when and how to press the button. For children under 8, or for children with cognitive impairment/developmental delay an NCA is more appropriate. This is a guide only and there may be children under 8 who would be able to use a PCA effectively.
Dedicated anti-syphon/reflux infusion lines with maintenance fluids to ensure patency of cannula.
Morphine / Oxycodone syringe should be prepared as
1mg/kg in 50mls 0.9% Saline
20micrograms/kg/ml; maximum 50mg in 50mls (1mg/ml)
Please refer to this document (Sharepoint link) for practical guide to setting up NCA in neonatal population.
Troubleshooting/changing settings
- In pain
- Side effects – itch/n&v/ileus
- Resp depression/sleepiness
Children on PCA/NCA should have hourly pain scores documented on their PEWS chart or on PCA/NCA chart. A trend of escalating pain scores should trigger a call to APRS (84319).
Other things to check/consider include:
- Patency of IV access
- Is PCA/NCA pump programmed correctly and working?
- Has the patient had adjuvant analgesia (should be prescribed regularly)?
- Do they need a loading dose/titration?
- Consider increasing background, increasing bolus dose or reducing lockout – this should only be done by the APRS/on call anaesthetist
- Low threshold for re-review by surgical/parent team if pain out of proportion or new.
All patients with NCA/PCA should be prescribed at least PRN anti-emetics. Anti-emetic guidance is provided later in this document.
Itch can be managed with either low dose naloxone (1mcg/kg) or piriton (250mcg/kg – max dose 2.5mg IV)
Ileus is commonly seen following abdominal surgery and use of post op opiates can compound this. We advise early conversion to Oxycodone as this is associated with a lower incidence of ileus. Conversion to oxycodone may also effective for children with nausea/vomiting and/or itch.
If a child on an opiate infusion is excessively sleepy, or with a RR <10, the infusion should be stopped and the ward/parent team should be called to review. As part of the standard ABC assessment of an unwell child, naloxone should be administered.
Dose:
- For Severe (life threatening) respiratory depression = 400mcg
- For sedation/mild respiratory depression/itch = 1mcg/kg
This can be repeated at 5 minute intervals for 5 doses, maximum dose 2mg. Ideally given IV but can be given IM or SC if these routes are available. By IM and SC routes, both the dose and the frequency are the same as above.
Consider smaller dosing initially in children at risk of withdrawal, or in children who will continue to need opiates (post-operative care, palliative care, mucositis, sickle cell crisis).
Oral Morphine Solution (Oramorph): immediate release preparation, and the most commonly used and prescribed in RHC. It can be prescribed for children post op, to facilitate painful procedures, and in children with painful medical conditions who don’t require an opiate infusion or who don’t have IV access.
Guideline starting dose 100-300mcg/kg 4-6hourly
If under 1year consider starting 50mcg/kg 4-6 hourly
This can be given more regularly if required, but prescribing outwith the guideline doses or frequencies above should involve discussion with the acute pain service.
Oramorph is frequently given to patients to take home, particularly after more painful (but day case) surgery.
Immediate release morphine is also available in tablet preparation (sevredol), with the same doses as above.
Slow release/modified release preparations of morphine are available as MST. Children may come into hospital on MST in which case it should be continued to avoid withdrawal, or converted to parenteral morphine if NBM or not tolerating oral diet.
Oxycodone: Similarly oxycodone is available in liquid form and as immediate release (shortec/oxynorm) or modified/slow release (longtec). These are often prescribed as a step down from oxycodone PCA/NCA/Infusion and as a routine part of post-operative analgesia for children having NUSS bar insertion or complex orthopaedic surgery. These children go home with a combination of regular slow release oxycodone, plus breakthrough immediate release, and are followed up by the acute pain service.
Codeine/DHC- NOT ROUTINELY USED in RHC. This is due to the risk of respiratory depression in children who are ultra-fast metabolisers (of codeine to morphine as active metabolite). As a result, codeine is not used in children under 12 and for all children under 18 following tonsillectomy for OSA. Children may be continued on codeine/DHC if transferred on it from other centres/using pre-admission. Guidance for the Administration of Codeine and Alternative Opioid Analgesics Nov2013.pdf (apagbi.org.uk)
If unresponsive or respiratory depression (RR <10, or <20 for an infant)
- ABC – follow BLS algorithm
- Give O2, call for help
- Naloxone given by repeated IV bolus (can be repeated every 5 mins)
- Dose – for severe (life threatening) respiratory depression = 400mcg (IV, IM or SC)
- Infusion if needed, starting at 10mcg/kg/hr
Intrathecal opiates are given for all NUSS bar insertions and in some children undergoing major colorectal/abdominal/orthopaedic surgery. In most cases this is diamorphine at a dose of 300-400mcg (5-10mcg/kg) given as a single injection. These children can have a PCA post op, but should not have any background infusion of opiate for at least 12 hours.
They can have short acting oral opiates - in the case of NUSS bar insertion this is Shortec (short acting oxycodone). Children post NUSS bar insertion will also be prescribed 12 hourly Longteq, with the first dose given the following morning after surgery.
Post-surgery these children should be prescribed naloxone as below, and monitored carefully for respiratory depression. They require hourly Obs and continuous oximetry with oxygen prescribed. They should be nursed in a central 4 bedded bay where possible.
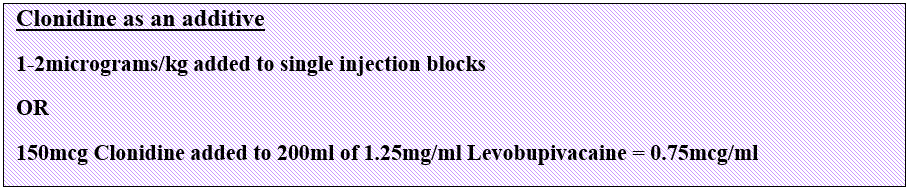
Clonidine is an α2 agonist which works centrally as an analgesic. It can be given orally, IV, or transdermally, as well as being added to neuraxial or peripheral blocks to prolong the duration of action. It has both sedative and analgesic properties as is commonly used as a premedication.
Clonidine can be given orally or NG at a dose of 1-5mcg/kg TDS.
Infusion – in RHC, clonidine infusions are only used in critical care and theatres, as continuous monitoring and airway support is required. The dose by infusion is 0.1-2mcg/kg/hr, titrated to effect. For infusions lasting 5 days or more, clonidine should be weaned slowly over 2-3 weeks. This can be by conversion to oral and a reduction in dose and then frequency. Weaning too quickly or abrupt withdrawal can result in rebound hypertension.
Ketamine is an NMDA receptor antagonist which has anaesthetic and analgesic properties. It produces a dissociative anaesthesia, and analgesia partly by an interaction at opioid receptors. At high doses it has local anaesthetic properties, by Na channel blockade.
It can be used as an oral or i.m premedication (dose up to 5mg/kg).
By infusion, it is used commonly in children with Sickle Cell Crises, mucositis, and as a third line agent in treatment of acute post-operative pain. It is almost exclusively used in 2A (schiehallion) and PICU.
Children on Ketamine infusions need to be centrally monitored, with continuous saturation monitoring and hourly observations.
Ketamine 10mg/kg in made up to 50ml N/Saline (max 500mg/50ml) and run at a rate of 1-5ml/hr. Equivalent mg/kg rates are found in the following guidance:
Intravenous Ketamine (Sharepoint link)
Some children receiving ketamine can experience hallucinations or dysphoria, which can be distressing. A quiet environment with minimal stimulation is advised. A small dose of morphine may also help to relieve this side effect. All children on ketamine infusions will be reviewed by the Acute Pain team at least twice per day.
Epidurals are used for intra- and post-operative analgesia following complex orthopaedic surgery, colorectal surgery, urological surgery and thoracic surgery. The prescription chart will have details of insertion including depth to space, length of catheter in space, any complications and initial dose given. The inserting clinician will also make up the bag and start the infusion, calculating the rate as shown below.
Epidural infusions can be continued for post-operative analgesia for a maximum of 72 hours, unless tunnelled. After this time, they are removed by APRS or Anaesthetics.
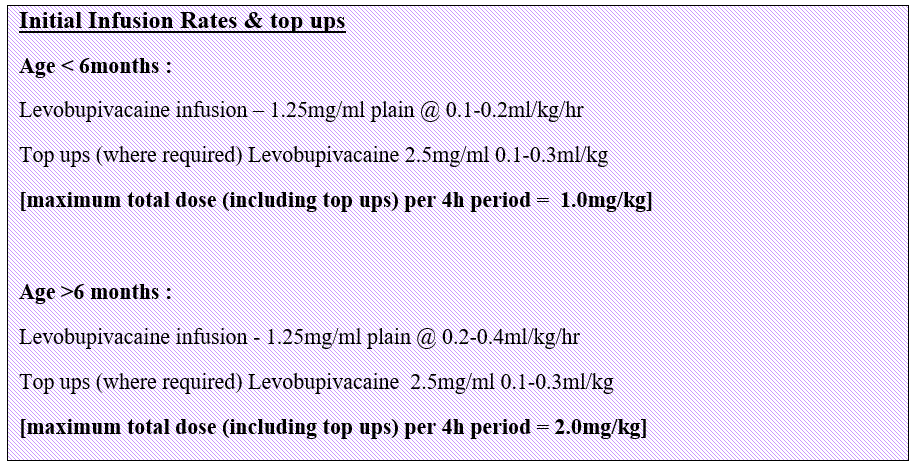
Top ups are given by an anaesthetist and can be useful to increase the height of the block and achieve effective analgesia. Prior to top up, block level should be checked. After top up, nursing staff are asked to check BP, HR, RR and SPO2 every 5 mins for 15 mins. After this time, the anaesthetist should check the block (motor and sensory level) and pain score. The aim is to achieve a block height sufficient to cover the wound, with good analgesia and preservation of motor power. There may be some motor block after top up with 0.25% levobupivacaine. If this persists the patient should be re-reviewed.
Additives to epidural solutions:
In specific cases, an additive may be mixed with levobupivacaine to prolong the analgesia from a single dose or to increase the dermatomal coverage of the block. This will be done by the theatre anaesthetist and any subsequent bags by APRS or by the on call anaesthetist.
Guideline for motor block observations and epidurals (Staffnet link)
LA toxicity can present biphasically: first with neurological signs such as agitation, seizures and loss of consciousness, progressing to cardiovascular instability with bradycardia, conduction disturbances, asystole/VT.
Management is as per AAGBI LA Toxicity guidelines:
Depending on the epidural insertion level, a high block presents progressively with increasing breathlessness/WOB (as intercostal muscles are blocked), and progressive hypotension followed by bradycardia (blockage of cardiac accelerator fibres).
Stopping the epidural should be a priority, alongside ABC assessment and management, oxygen, fluids, and targeted treatment to manage hypotension and bradycardia. This may include:

In children with an epidural indwelling catheter, on LMWH thromboprophylaxis, concomitant treatment with antiplatelet medication (e.g. NSAID’s) should be avoided if possible.
Removal:
In children on ONCE DAILY dose LMWH thromboprophylaxis the removal of the epidural should be at least 10 hours after the last dose of LMWH.
Next LMWH Dose:
In children on ONCE DAILY dose LMWH thromboprophylaxis, the next dose of LMWH should be given at least 4 hours after the removal of the epidural catheter.
Removal:
In children receiving TWICE DAILY LMWH thromboprophylaxis the removal of the epidural should be at least 8 hours (2 half-lives) after the last dose.
Next LMWH Dose:
In children receiving TWICE DAILY LMWH thromboprophylaxis, the next dose of LMWH can be given 4 hours after the removal of the catheter, so the BD prescription times do not need to be changed.
If a bloody tap occurs during the placement or removal of the epidural catheter, the event should be recorded in the notes, the consultant must be informed, greater degree of vigilance exercised,(please refer to policy for motor block density) and the next dose of anticoagulant delayed for 24 hours.
In patients receiving LMWH, monitoring and observation of neurological status should be continued for at least 24 hours after the catheter removal and recorded in the notes
NEONATES: Before removing epidural or caudal catheters in neonates, use caution as some neonates may be at risk of post-operative coagulopathy. Seek senior advice prior to removal if concerned.
AAGBI Regional Anaesthesia and Patients with Abnormalities of Coagulations
Direct infiltration of a wound with LA blocks noxious afferent pain pathways, and can provide anaesthesia without risks or complications of neuraxial blockade. Catheters can be placed in any surgical wound and in RHC, catheter through needle kits are available (PAJUNK) in a variety of sizes. Catheters used can be 100mm, 150mm and epidural catheters. The catheters are multi-holed and the system is designed to infiltrate uniformly across the length of the holes. The entire length of the perforations should be within the wound, to avoid significant leakage. The catheters are inserted in theatre and under direct vision by the surgeons. The responsible anaesthetist then fills the PAJUNK elastomeric pump as per RHC Guidelines below:
Clinical guideline for use of Pajunk wound infusion catheters (Staffnet link)
The elastomeric pump is filled with 350ml 0.125% L-Bupivacaine, and the device adjusted to give a rate in ml/hr (3, 5 or 8ml/hr). All devices are single use and can’t be refilled. For wounds which require bilateral nerve blockade (such as midline laparotomy), 2 catheters are inserted, and a Y connector used to connect to a single elastomeric pump.
The catheter (or catheters) can remain in place for 48 hours post op.
Consider –
Peppermint Water BP [not licensed for use in children less than 12 years, however may be considered for use within RHC]
Do not give to children under 3 months
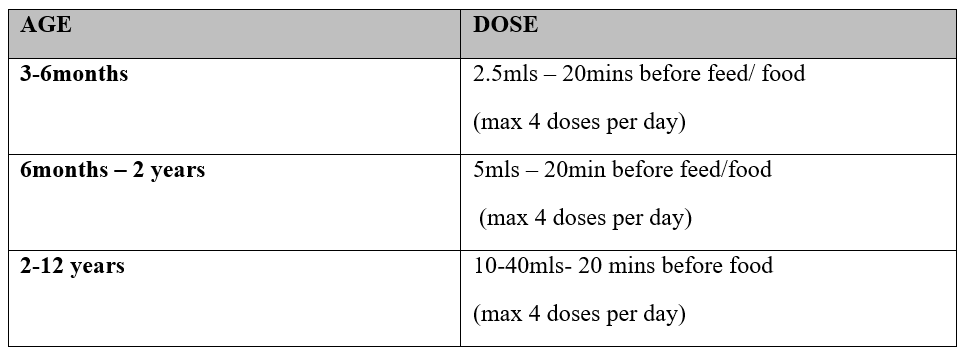
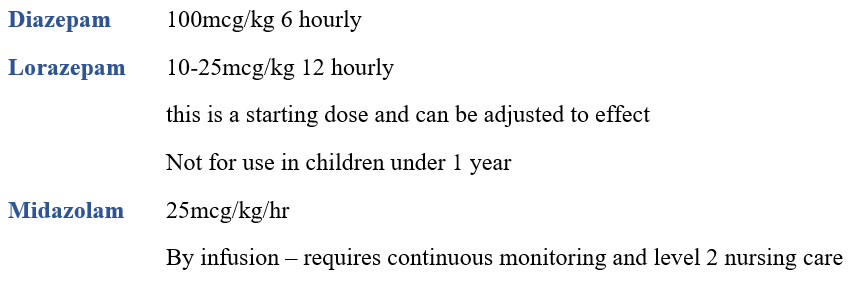
Muscle spasms are common following complex orthopaedic surgery (e.g tendon lengthening, osteotomy) and children with Cerebral Palsy are particularly at risk of post-operative spasms. Effective post-operative analgesia often includes a neuraxial or regional blockade. The addition of clonidine to regional blockade can reduce the incidence of painful spasms. It is also advisable to start these children on an anti-spasmodic which can be:
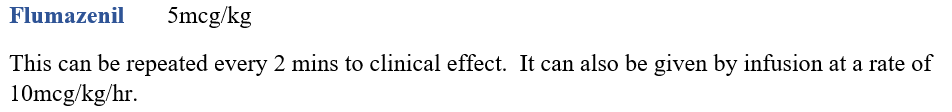
As for opiate antagonism, benzodiazepines can be antagonised in the presence of respiratory depression or unresponsiveness. The treatment is:
It is often very worthwhile considering non-pharmacological techniques as adjuncts to pain management. Dependent on the age of the child, things to consider are:
- Skin to skin
- Sucrose (Oral sucrose for procedural pain)
- Swaddling/wrapping
- Hot/cold therapy
- Play therapy
- Distraction
- Vibration
- TENS
APA Post op nausea and vomiting guideline
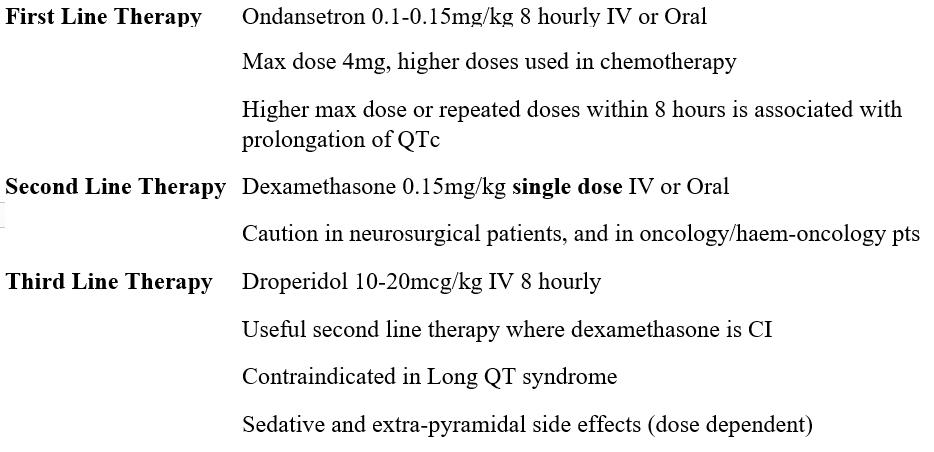
There is no/limited evidence on the efficacy of Cyclizine in the management of PONV in children.
There is good evidence that combined therapy of ondansetron plus dexamethasone is more effective than either single therapy in the prevention of PONV in children.
Please follow links below to access RHC guidelines on management of:
ADENOTONSILLECTOMY (SAME DAY SURGERY)
- Link to follow
NUSS BAR/RAVITCH PROCEDURE
- Pain Management Flow Chart For Chest Wall Surgery Aug 2022 (Sharepoint link)
DRESSING & DRAINS
- RHC Entonox Guideline (Staffnet link)
COMPLEX ORTHOPAEDIC SURGERY
- Pain Mgt Complex Orthopaedic Surgery (Sharepoint link)
- Wong, D. and Baker, C.: Pain in children: comparison of assessment scales, Pediatric Nursing, 14(1):9-17, 1988
- Malviya S et al: The revised FLACC observational pain tool: improved reliability and validity for pain assessment in children with cognitive impairment. Paed Anaes, 16(3) 2006.
- https://bnfc.nice.org.uk/drugs/paracetamol/
- Zempsky WT, Bhagat PK, Siddiqui K. Practical Challenges-Use of Paracetamol in Children and Youth Who are Overweight or Obese: A Narrative Review. Paediatr Drugs. 2020 Oct;22(5):525-534. doi: 10.1007/s40272-020-00417-z.
- Paracetamol SCH. Practical Guideline. March 2020.
- APA RCPCH Guidance for the administration of codeine and alternative opioid analgesics in children.
- Anirudda Pai, MD DNB FRCA, Mark Heining, MD FRCA, Ketamine, Continuing Education in Anaesthesia Critical Care & Pain, Volume 7, Issue 2, April 2007, Pages 59–63.
- Intravenous Ketamine – RHC Guidance for nursing staff. Pain Management Service RHSC Glasgow 2010.
- AAGBI Management of Severe Local Anaesthetic Toxicity. 2010.
- Association of Paediatric Anaesthetists of Great Britain and Ireland. Guidelines on the Prevention of Post-operative Vomiting in Children 2016.
Last reviewed: 26 September 2023
Next review: 30 September 2026
Author(s): Dr Alana Kirkwood, Consultant Paediatric Anaesthetist and Lead for Acute Pain Service, RHC
Version: 21
Author Email(s): alana.kirkwood@ggc.scot.nhs.uk
Approved By: Anaesthetic Advisory Group
Document Id: 1119

