Conscious sedation in the Cardiac Catheterisation Laboratory RHC, Glasgow
exp date isn't null, but text field is
Conscious sedation is commonly used for electrophysiological procedures within the adult sector and in recent years has been implemented for selected adolescent patients in Royal Hospital for children (RHC), Glasgow.
The electrophysiological procedures for which conscious sedation is employed include diagnostic and ablation procedures for cardiac arrhythmias and the insertion of implantable electronic loop recorders.
The goals of procedural sedation and analgesia include administering the lowest dose of medication to:
- Maintain patient safety and welfare
- Minimise physical pain and discomfort
- Control anxiety, minimise psychological trauma, and maximise amnesia
- Control behaviour and movement to allow safe performance of the procedure
Conscious sedation should be performed by specialised nurses, who have received appropriate training, under the supervision of the procedural Interventional Consultant Cardiologist and with back up support of consultant anaesthetist if required.
- The Cath Lab nurse must have successfully completed the RHC approved intravenous competencies.
- Only nurses who have undertaken instruction in the use of this protocol and successfully completed the Cath Lab conscious sedation competency can administer fentanyl/midazolam using this technique.
- Administration should be undertaken under the supervision of the Consultant Cardiologist trained in the principles and practice of conscious sedation.
- A Consultant Anaesthetist should be informed that procedure is taking place and be available for advice
- ASA (American Society of Anethesiology) III and IV
- Anatomic airway abnormalities, obstructive airways disease (eg. moderate to severe tonsillar hypertrophy, obstructive sleep apnoea) or any respiratory depression
- Known hypersensitivity to fentanyl citrate, other morphinomimetics or muscle relaxants
- Concurrent administration with monoamine oxidase inhibitors or within 2 weeks of their discontinuation
- Brain trauma/ raised intracranial pressure
- Known hypersensitivity to naloxone
- Known hypersensitivity to benzodiazepine or flumazenil
- Known hypersensitivity to ondansetron
- BMI > 30
- ASA I and II
- Age >12 years, patient and parent fully informed, consent from parent AND patient
- Confirming fasting status
- If any airways concern, involve an anaesthetist
- 18.5 < BMI < 25. If 25 < BMI <30, ask advice
- A normal healthy patient
- A patient with mild systemic disease
- A patient with severe systemic disease.
- A patient with severe systemic disease that is a constant threat to life
- A moribund patient who is not expected to survive without the operation
For fasting instructions please refer to Cardiac Fasting Guideline
NHSGGC - Fasting guidance for children with Congenital Heart Disease
- Drugs prescribed by consultant cardiologist
- Cardiac Cath Lab nurse to note any allergies or drug sensitivities and the appropriate fasting time
- Patient to have two intravenous cannulae inserted in ward.
- Cannulae to be flushed with 5mls sodium chloride 0.9% to check their patency
- Commence patient on 2 litres of oxygen via nasal cannula which will continue throughout procedure
- Monitor exhaled CO2 throughout procedure
- Commence ECG, oxygen saturation and blood pressure monitoring on patient’s arrival in Cath Lab and continue throughout the procedure.
- The patient’s level of consciousness will be assessed as well.
The patient can bring an electronic device they can use with headphones throughout the procedure.
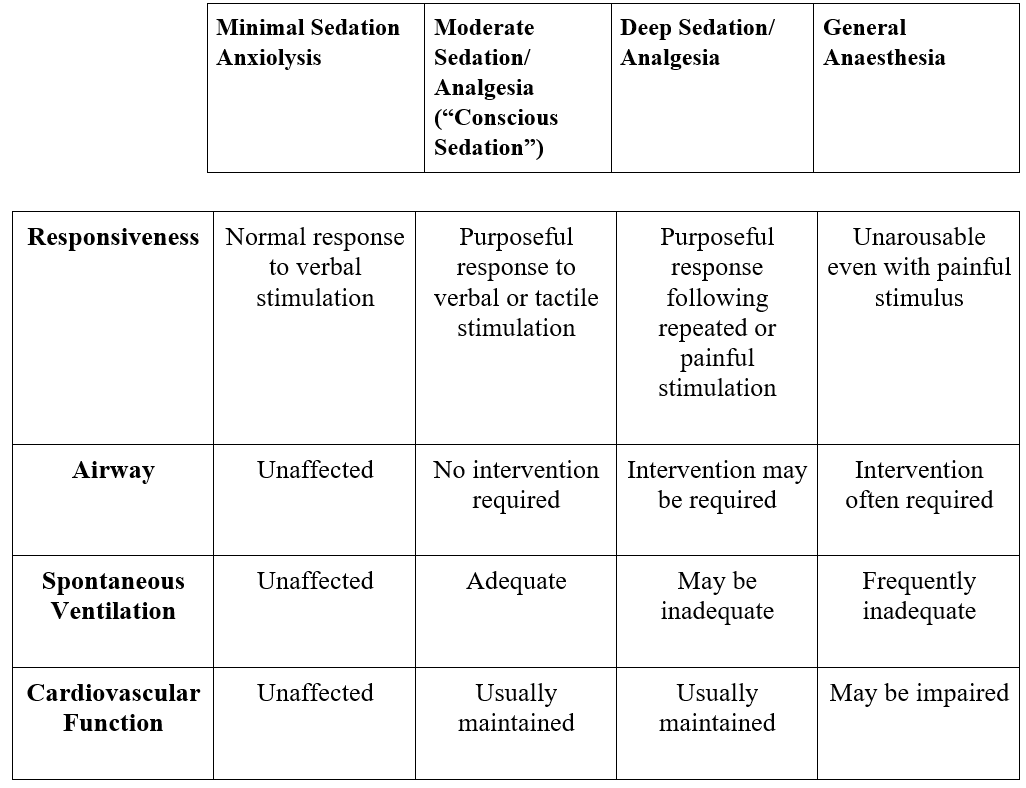
The terms moderate sedation and procedural sedation are now used interchangeably.
Sedation exists along a continuum that progresses from a state of minimal sedation to general anaesthesia.
Procedural sedation and analgesia is a drug-induced depression of consciousness during which patients respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation (reflex withdrawal from a painful stimulus is not considered a purposeful response). No interventions are required to maintain a patent airway, spontaneous ventilation is adequate and cardiovascular function is maintained.
Equipment and environment
Sedation should be administered in an environment where constant monitoring can be provided.
Resuscitation equipment must be available (oxygen with an appropriate size mask and reservoir, oropharyngeal airway, LMAs (Laryngeal Mask Airway), endotracheal tubes, suction catheters, resuscitation drugs). Flumazenil and Naloxone must be readily available.
Monitoring equipment - see below
Procedural monitoring
Before sedation is given, standard monitoring of patients undergoing Electrophysiology studies and Radiofrequency ablation includes recording:
- Oxygen saturation
- Heart rate
- End-tidal CO2
- Blood pressure
- Respiratory rate
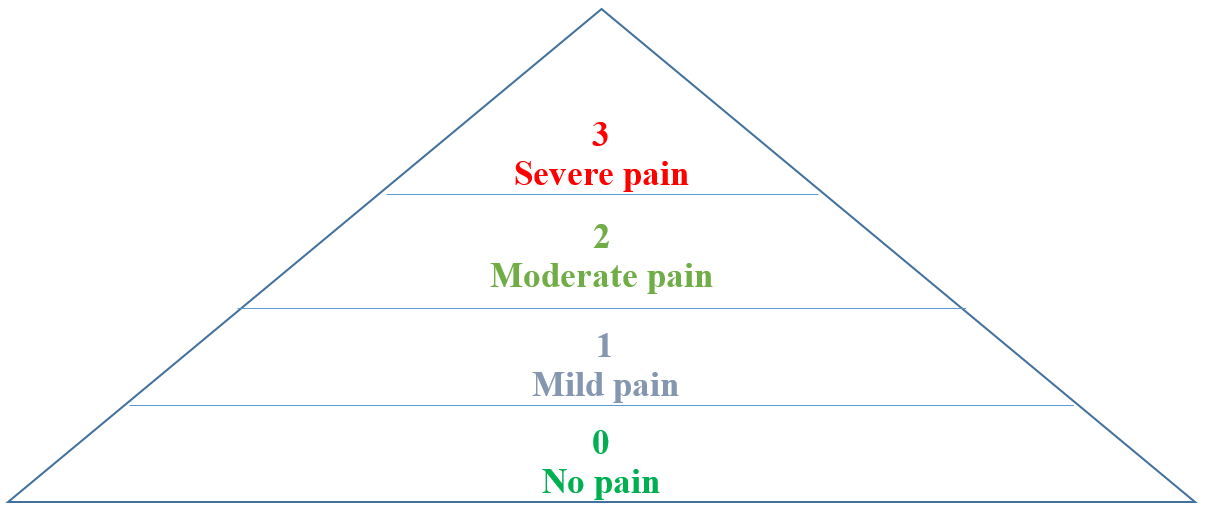
Before the administration of any sedative, assess the patient’s baseline sedation level and establish baseline capnography. If sedation scores above 0, do not administer any medications. Investigate possible causes of sedation e.g. other medications and discuss findings with the Consultant Cardiologist.
During the procedure:
- Oxygen saturation
- Heart rate
- End-tidal CO2
- Blood pressure
- Respiratory rate
- Sedation level
- Pain threshold and action taken as appropriate
Should be monitored continuously during the procedure and documented every 15 minutes. This monitoring should continue until the patient is stable after the procedure. All observations should be recorded on Anaesthetic chart.
Combinations of carefully titrated sedative, analgesic and hypnotic medications alter a patient’s level of consciousness and enhance cooperation. However, sedative and analgesic medications also may produce synergistic effects which may lead to deep sedation to general anaesthesia. Successfully producing a sedate, analgesic state and minimizing complications (respiratory distress, cardiovascular depression and hypoxemia) requires an understanding of these medications as well as the reversal agents that may be needed if the level of sedation becomes deeper than intended.
MIDAZOLAM
Midazolam is a benzodiazepine used for inducing moderate sedation. Dose: 0.05-1 mg/Kg. Peak effect: 3-5 min. Duration: 30-60 min.
- Midazolam 1mg/ml should be drawn up into a 2 ml syringe to give 2mg in 2mls ready for administration.
- Ensure syringe is labelled correctly
- The midazolam should be administered neat IV
- The initial dose of 2mg should be administered 5 to 10 minutes prior to the insertion of vascular sheaths.
- Reduced doses may be required in patients weighing less than 50kg
- The maximum titrated dose the patient may receive within the scope of these guidelines is 5 mg of midazolam administered in increments according to the prescription chart.
FENTANYL
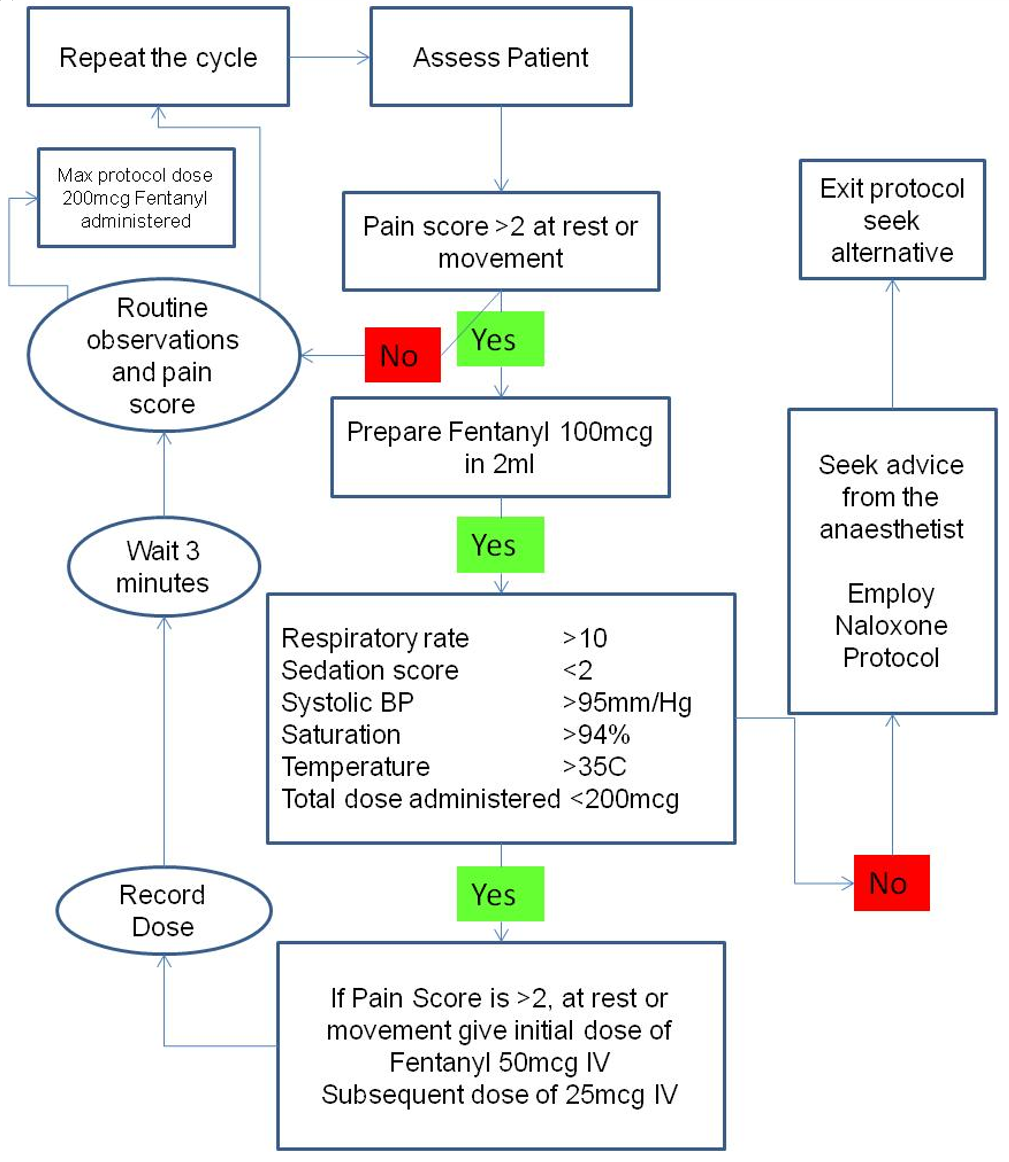
Fentanyl is a strong opioid that is being used as analgesia during the procedure. Dose: 1-5 mcg/kg. Maximum respiratory depression occurs within 7-10 min after IV administration.
- Fentanyl 50 mcg/ml should be drawn up in a 2 ml syringe which gives 100 mcg in 2 ml
- Ensure syringe is labelled
- The fentanyl should be administered neat as an IV
- Administer the first 50 mcg at the start of the procedure.
- A reduced dose may be required in those less than 50 kg
- Subsequent 25 mcg doses may be given as required for analgesia
- The maximum titrated dose a patient may receive is 200 mcg administered in increments according to the prescription chart
- If maximum dose has been given and patient complaining of pain, seek anaesthetist’s advice.
FLUMAZENIL
Flumazenil is used to reverse unwanted side effects of benzodiazepines such as midazolam. It is available in an ampoule of 500 micrograms in 5 ml.
- Flumazenil (100 micrograms/mL) should be drawn into a 2 mL syringe (200 micrograms in 2 mL) ready for administration.
- Flumazenil is administered undiluted.
- If the respiratory rate falls below 10 breaths per minute call an anaesthetist.
- If the Anaesthetist and/or Cardiologist is not available immediately the Cath Lab nurse is permitted to administer flumazenil as per this protocol.
- The initial dose of 200 micrograms administered over 15 seconds. If the desired degree of consciousness is not obtained within 60 seconds, a second dose of 100 micrograms can be administered. The usual dose is 300 to 600 micrograms, but may be adjusted according to the patient's response.
- If the patient condition remains stable, wait 5 minutes and reassess respiratory rate.
- If the respiratory rate is still below 10 breaths per minute a further dose of 1 mL (100 microgram) of flumazenil should be given
- Wait for another 5 minutes, reassess and administer a further dose of 1 mL (100 microgram) of flumazenil if required.
- A total of 20 mL (2000 micrograms) of flumazenil may be given if required in 1 mL (100 microgram) incremental doses over a total period of 20 minutes.
Do not give further doses of benzodiazepines.
Flumazenil should not be given to an epileptic child who had been on long term benzodiazepine treatment, as it may precipitate a withdrawal convulsion.
No patient shall be discharged from Cardiac Catheterisation Lab before being assessed by the Anaesthetist or Cardiologist in charge of the patient’s care.
Patients should be sent to recovery for at least 20 minutes after giving flumazenil to check for signs of re-sedation.
The duty anaesthetist should be informed.
NALOXONE
Naloxone is used to reverse the unwanted effects of opioids such fentanyl
- Naloxone 400mics /ml should be diluted with 3mls of 0.9% Sodium Chloride to give Naloxone 100mic/ml
- Ensure the syringe is labelled correctly
- If the respiratory rate falls below 8 breaths per minute call the Anaesthetist and responsible Cardiologist.
- If the Anaesthetist and/or or Cardiologist are not available immediately the Cath Lab nurse is permitted to administer naloxone as per this protocol.
- Administer 1 ml (100 microgram) of naloxone intravenously.
- Provided the patient remains stable, wait for two minutes and reassess respiratory rate.
- If the respiratory rate is still below eight breaths per minute a further dose of 1 ml (100 microgram) of naloxone should be given.
- Wait another two minutes and reassess the respiratory rate, administer a further dose of 1 ml (100 microgram) of naloxone if required.
- A total of 400 microgram of naloxone may be given if required in divided incremental doses of 100 microgram in a single session. If further doses are required, contact the duty Anaesthetist.
Do not give further doses of fentanyl or opioids for at least 30 minutes following administration of naloxone.
No patient shall be discharged from Cardiac Catheterisation Lab before being assessed by the Anaesthetist or Cardiologist in charge of the patient’s care.
Patients sent to Recovery for at least 20 minutes after giving naloxone to check for signs of re-sedation.
The duty Anaesthetist should be informed.
THE USE OF ANY REVERSAL AGENT MUST BE LOGGED IN DATIX AS AN ADVERSE EVENT AND IMMEDIATELY ESCALTED TO CATH LAB SENIOR CHARGE NURSE
ONDANSETRON
Ondansetron is a 5-HT3 receptor antagonist used to prevent nausea and vomiting during the procedure. Dose: 0.15 mg/kg
- Ondansetron 2 mg/ml should be drawn into a 2ml syringe neat ready for administration.
- Ensure syringe is labelled correctly
- Administer 4 mg of Ondansetron followed by a flush of 0.9% sodium chloride, 5 min prior to procedure commencing
- The maximum dose the patient may receive is 8 mg per Cath Lab session
- If maximum dose has been administered and patient remains nauseous then seek anaesthetist’s advice re further antiemetics
PARACETAMOL
Paracetamol has a central analgesic effect and can be used alone or in combination with opioids. Dose IV: 15 mg/kg every 4-6 hrs (bodyweight 10-50 kg); 1 g every 4-6 hrs (body-weight 50 kg and above)
OXYGEN
Administer oxygen at a flow of 2 litres via nasal cannula whilst monitoring CO2
Recording of Medication
Record the drug, dose, route and time given in the patient’s prescription chart
Preparation, administration and destruction of the fentanyl syringe must be recorded in the controlled drug register.
If patient requirements suggest that the limits described within this protocol are likely to be exceeded, the Anaesthetist supporting the procedure must be called to review
Administration of sedative and analgesic agents carries some risks and complications that include:
- Respiratory depression
- Loss of consciousness
- Loss of airway
- Laryngospasm
These medications alter airway muscle activity, which can lead to airway obstruction. Signs and symptoms include:
- increased respiratory effort
- sternal retraction
- rocking chest motion (not in Sync with respiratory effort)
- inspiratory stridor
- hypoxemia
- hypercarbia
- absence of breath sounds
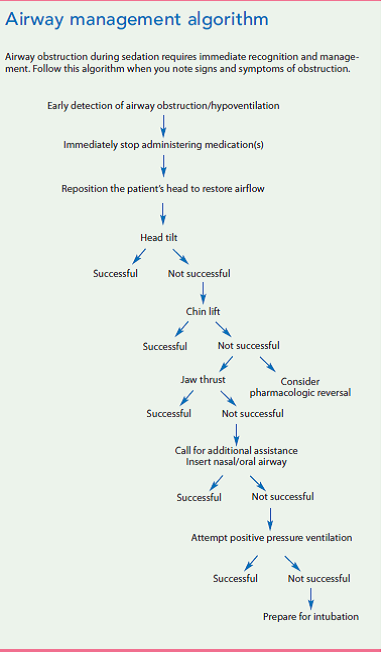
Use sedation airway management algorithm if airway obstruction and respiratory compromise occur during procedural sedation (see Airway management Algorithm).When an obstruction is identified, an immediate consultation with an anaesthetist for additional airway support and possible intubation should be requested.
Whilst awaiting Anaesthetist’s attendance, speak to and touch the patient to assess the level of consciousness and stimulate them. If these efforts aren’t successful and do not relieve the obstruction, use the lateral head tilt. This manoeuvre moves the head from a neutral to a lateral position in an attempt to provide partial or complete relief.
If head tilt is not successful, try the chin lift, which permits anterior movement of the mandible through superior displacement of the chin. This manoeuvre, combined with hyperextension of the head and neck and forward displacement of the mandible, will elevate the soft tissue anteriorly.
If verbal or tactile stimulation, head tilt, and chin lift do not relieve the airway obstruction, the patient has entered a state of deep sedation or general anaesthesia. If obstruction isn’t relieved and airflow restored, oxygen desaturation and hypoxemia will ensue. Next try the jaw thrust manoeuvre.
If jaw thrust does not relieve the obstruction, consider pharmacologic reversal.
A yearly audit on quality of conscious sedation is required. It should contain the following metrics:
- Number of reversal agents required/per number of patients sedated
- Number of occasions where escalation to senior anaesthetist was requested/per number of sedated patients
- Total dose of midazolam or fentanyl given (median/mean across patients requiring these drugs)
- Patient experience
- Operator experience
Last reviewed: 10 March 2022
Next review: 28 February 2026
Author(s): Lisa Kennedy, Karen McLeod, Stefania Leone
Version: 1
Approved By: Scottish Paediatric Cardiac Service

