Complex care management for children and young people with Exceptional Health Care Needs protocol
exp date isn't null, but text field is
Objectives
1.1 Scope and Purpose of this Protocol
This protocol is designed to support effective collaboration between health teams across maternity, family nurse partnership, neonates and children and young peoples in patient and community services in order to support robust complex care management for children with exceptional health care needs. Specifically around:
- Delivery of safe effective ongoing packages of care.
- Support and coordination of care during complex discharges.
- Effectively coordinating care during key transition periods.
It aims to fully involve children, young people and their families/carers in the process to ensure that they receive appropriate assessment, planning and information about the arrangements for ongoing care and support.
It aims to enhance collaboration by professionals across children’s health services, working together, sharing together and learning together in the provision of excellence in care and pursuit of improved outcomes for children, young people and their families.
It aims to fully embrace the principles of Getting it Right for every Child (GIRFEC), which is our national approach to delivering the United Nations Convention of the Rights of Children (UNCRC), and which has been incorporated into Scots law.
It aims to firmly embed care management practice as a transaction which upholds the principles of the national approach to improving outcomes for children and their families.
The associated Learn pro module is now LIVE, is called GGC:311 Complex Child Protocol and is listed under Role specific Mandatory Modules.
1.2 Children with exceptional healthcare needs (CEN) are described by the Managed Clinical Network using assessment criteria based upon 6 areas of need. These are:
- Learning and mental function
- Communication
- Motor skills
- Self care
- Hearing
- Vision
- Social and emotional health and well being
A child or young person (up to the age of 19) is defined as having exceptional healthcare needs if they
- Have severe impairment recorded in at least 4 categories together with enteral/parental feeding Or
- Have severe impairment recorded in at least 2 categories and require ventilation/CPAP and
- The impairments are sustained and ongoing or expected to last for more than 6 months.
1.3 Complex Discharges can be defined as:
Babies, Children and young people with exceptional health care needs resulting in increased level of needs and requirements for ongoing coordination and planning of care, particularly at discharge and during periods of transition. Care management may informed by defined pathway or clinical protocols and be managed jointly by ward-staff and a clinical team within a specialty who bridge the gap between hospital and community. Home and self-care needs are clearly defined and discharge can be planned within an expected period of time.
Or
Babies, children and young people with exceptional health and care needs, where additional vulnerabilities may coexist within the child’s family or wider environment. High level of dependency and significant risks associated with home care. Input and support is likely to be required long-term. Multi-disciplinary/multi- agency input is needed to coordinate discharge, create a single child’s plan, support implementation and review of the plan, and ensure that the child’s needs are met on discharge and in the longer term.
This protocol applies to all health professionals working in acute maternity, family health partnership, paediatric, neonatal inpatient settings as well as community specialist children and families’ service and universal services such as health visiting and school nursing.
(To note, that where the protocol refers to children and young people, it assumes babies and infants as well.)
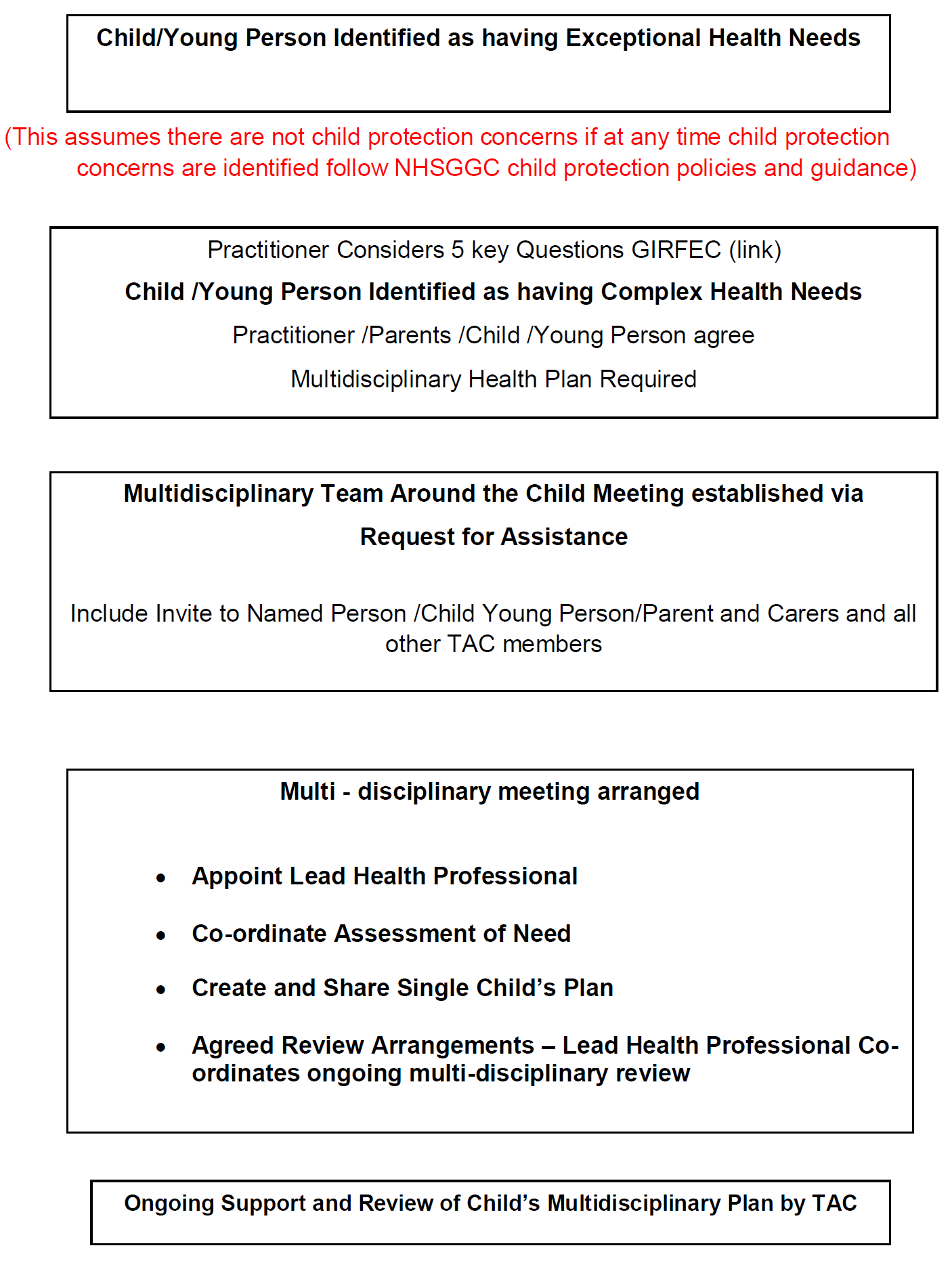
2.1 Care Planning and Co-ordination in the context of the GIRFEC Practice Model
This protocol describes the framework within health for the safe and effective care management of babies, children and young people with complex care needs and/or associated family related vulnerabilities.
Developed in line with the principles of Getting it Right for Every Child1 this framework assumes family centredness with the child and family/carers at the heart of decision making, and included and involved at all points in the patients journey. Getting it Right for Every Child (GIRFEC) is the national multi-agency approach to improving outcomes for children and young people in Scotland. NHSGGC is committed to delivering the principles of GIRFEC throughout children’s health service. Full detail of GIRFEC can be found in the following link: http://www.scotland.gov.uk/Topics/People/Young-People/gettingitright.
It provides clarity of duties and responsibilities for health professionals in developing a comprehensive child’s healthcare plan which is coordinated and provides ongoing review and assessment.
It includes the Antenatal Universal Pathway developed across Maternity, Family Nurse Partnership and Universal Health Visiting Services, based upon GIRFEC principles. (Appendix 1)
This protocol introduces the concept of and circumstances where there is a requirement to appoint a Lead Health Professional whose role is to ensure that planning and delivery of complex health care, ongoing and particularly at discharge and times of transition remains robust and coordinated.
It applies GIRFEC principles in identifying both a Lead Health Professional role and multidisciplinary team known as the Team around the Child (TAC).
It enhances the support to children, young people and families provided by the Named Person and enables a person centred care response to identified health needs.
Where another agency is involved with the child, young person or family and fulfils the role of the Lead Professional, the framework strengthens the health contribution to multiagency assessment and planning (via the role the Lead Health Professional) and ensures that complex heath care continues to be robustly planned and co-ordinated across all multidisciplinary health teams involved with the child or young person’s care.
It describes a pathway which ensures seamless transition through services applying the same model and principles throughout the patient’s journey.
Any pathway has to be flexible and responsive to fluctuating need. Assessment and identification of care management is not a binary process and must be seen in the context of multiple factors such as changing need and vulnerabilities, or at points of transition and transfer of care.
Information sharing between professionals and services is an essential component in the ongoing assessment and identification of need. (Appendix 2).
Robust communication between professionals must be diligently endorsed and applied throughout the patient’s journey.
Systems and processes must be in place which supports effective communications and information sharing.
Datasets must be agreed by services which enable effective care management as well as provide the ability to monitor outcomes.
It is the duty and responsibility of professionals to fully embrace the GIRFEC principles and undertake robust assessment of need based on wellbeing indicators and My World Triangle.
2.2 Named Person and Lead Health Professional Role
The Named Person Role
Every child and young person will have a Named Person. The Named Person will usually be a practitioner from a health board or an education authority, and someone whose job will mean they are already working with the child. The Named Person will act as the first point of contact for children, young people and families providing a central point of contact if a child, young person or their parent (s) want information or advice, or if they want to talk about any worries and seek support The Named Person can also, when appropriate, reach out to different services who can help and enable access to assistance more easily.
The role includes:
- Assessment of what children and young people need, within the context of their professional responsibilities
- Linking with the relevant services that can help them
And - Being a single point of contact for services that children and families can use, if they wish. The Named Person is in a position to intervene early to prevent difficulties escalating. This is an essential feature of a child centred approach to early intervention.
The role offers a way for children and young people to make sense of a complicated service environment, as well as a way to prevent any problems or challenges they are facing in their lives remaining unaddressed due to professional service boundaries. Their job is to understand what children and young people need, and quickly make the connection to those services that can help when extra help is needed.
The Lead Professional Role
There are some circumstances where children and young people’s needs involve two or more agencies working together delivering services to the child and family. Where this happens, in all cases, a Lead Professional will be needed. The Lead Professional becomes the person within the network of practitioners supporting the child, young person and family who will make sure that the different agencies work together and the help they are all offering fits together seamlessly to provide appropriate support for the child and family. The Lead Professional will have a significant role in working with other agencies to co-ordinate a multi-agency Child’s Plan.
Across the Local Authorities contained within Greater Glasgow and Clyde, Health, Education and Social work have agreed the following demarcations for identifying Named Person and Lead Professional responsibility:
|
Age and Stage |
Named Person |
|
Pre- Birth to 14 days old |
Health Visitor or FN |
|
Children aged 0-5 |
Health Visitor |
|
Children aged 5-16 |
Education Staff |
|
Children and Young Person |
Lead Professional |
|
All looked after children |
Social Work Services |
|
Children with complex health needs |
Children’s Services? |
|
Child Protection |
Social Work Services |
N.B. Family Nurses will also take on the role of the named person for those families enrolled on the Family Nurse Partnership Program until 2 years of age before transitioning to the health visitor.
2.3 The role and function of the Lead Health Professional
It is recognised as best practice to provide children and young people who have complex health needs and their and families with a ‘care coordinator’, identified from the body of health professionals providing care and support to the child and family. This care coordinator is known as the Lead Health Professional.
An LHP is appointed based upon assessment of need, and or the professional who has the most effective engagement and or therapeutic relationship with the child or young person and family
The role is to coordinate the key activities contained within a multidisciplinary healthcare plan.
The term Lead Health Professional describes a designated clinician within the team who has responsibility to co-ordinate the organisation of patient care activities to facilitate the appropriate delivery of the required health care services to a child or young person
The role exists to ensure our complex health service pathway processes are progressed timeously and efficiently, and to ensure the child, young person and family has a clear point of contact.
The role of LHP should augment the continuing role of the Named person recognising the need for enhanced coordination and access to a broad range of services to optimise care for children and young people with exceptional care needs.
2.4 Team around the Child (TAC)
- The TAC is comprised of the key professionals involved with the child and family. The LHP is identified from and by the membership of the TAC.
- The TAC is responsible for coordination of robust multi- disciplinary assessment of need, the creation, of a single child’s healthcare plan, co-ordination of delivery and evaluation of the impact of the child’s plan in addressing their identified needs, and improving their outcomes.
- For complex care management to be delivered a variety of professionals with the necessary competencies must work as a team to augment the role of GP, Universal and Primary Care Service. There will be a range of specialist skills within the members of the TAC.
- Professionals will engage with the child or young person ongoing /or at appropriate stages for the delivery of a specific intervention from an individual discipline.
- Health professionals will adopt collaborative working practices to facilitate joint appointments and visits with the child or young person, and their families and carers where appropriate, ensuring responsive service provision reflective of ongoing and changing needs.
Key Principles to:
- Provide services in accordance with local and national key performance indicators, recognised best practise, and other emerging targets.
- Provide care based on assessment of the child, young person and family’s needs, promoting the health and wellbeing of the child and family, and ensure social inclusion of the child and family supporting families to live ordinary lives.
- Act as a contact/link for the family and communicate with Named Person.
- Actively involve children and young people and their families, adopting What Matters to Me (WMTM) approach, together with their primary care team, in all decisions affecting them.
- Facilitate family and professional collaboration at all levels of service provisions
- Respect and honour the racial, ethnic, cultural, socioeconomic and gender diversity of the child, young person and family.
Key aims are:
- Provision of multi-disciplinary assessment, diagnosis and interventions based upon the guiding principles of Realistic Medicine.
- Seamless transition to new lead health professional when that clinical need has resolved and new presenting need emerges.
- Co-ordination and management of care
- Co-ordination and dissemination of information relating to the child or young person to multi-disciplinary and multi-agency meetings and professionals
- Provision of high quality family centred care and support
- Maximised health and quality of life outcomes for children and young people
- Onward referral and signposting where appropriate
- Effective transition planning
Essential Members of the Team around the Child Team:
- RHC Paediatricians
- Community Paediatricians
- General Practitioner
- Clinical Nurse Specialist
- Ward based Nursing Team
- Community Paediatric Nursing
- Health Visiting
- Family Nurse Partnership
- Mainstream School Nursing
- ASL School Nursing
- Hospital Allied Health Professionals
- Community Paediatric Physiotherapy
- Community Paediatric Occupational Therapy
- Community Paediatric Speech and Language Therapy
- CAMHS (where appropriate)
- Third Sector Providers (where appropriate)
In addition at transition to adult services, adult clinical teams will join the TAC and might include professional(s) from Mental Health, Learning Disability, Addiction, Acute and Community Adult Services.
2.5 Multidisciplinary Assessment and Care Planning by the TAC
The formation of a person centred single child healthcare plan requires gathering a range of information to inform the type and level of support required for the individual child or young person and the family based on robust assessment of need
This is the responsibility of the TAC and is coordinated by the LHP. Implementation and progress is reviewed via multidisciplinary Complex care coordination meetings for children and young people with CEN. The complex care co-ordination meeting will enable the development of a multidisciplinary assessment based upon professional assessments and facilitate the creation of a healthcare plan.
The meeting will:
- Coordinate a multidisciplinary assessment of the needs of the child or young person
- Develop a single child’s care plan
- Secure the views of the child or young person and their parents /carers
- Identify and agree the input of members of the MDT
- Implement the care plan, with clear timetable for planned review
- The child’s plan will explain what the expected outcomes are for the child within defined timescale, what actions are to be taken and by whom.
- The child's health plan is coordinated by a 'lead health professional': someone with the right skills and experience to make sure the plan is managed properly.
- Depending on the situation and the child's needs, the lead professional may also be their named person or a health professional who had key impact on their care. This can change over time but communication with the TAC must remain and be considered at each review point or as requested.
- The child and parent(s) will know what information is being shared, with whom and for what purpose and their views will be taken into account. (This may not happen in exceptional cases, such as where there is a concern for the saety of a child or someone else.)
- The parents/carers and child and young people must be active contributors to their plan with the views listed too and considered documented.
2.6 Request for Assistance
There may be occasions during the patient journey when the identified needs and indicator of risk change requiring alteration to the child healthcare plan. When this happens the Professional who identified the change invokes the Request for Assistance Procedure. (Appendix 3)
There are 4 criteria when the Request for Assistance procedure must be initiated:
- When a health professional, or a parent or young person themselves has identified that the child or young person’s needs are not being met by any current provisions or that they have new information or a concern which required multidisciplinary review.
- When a health professional considers discharge of the child or young person from service. (This should be done in conjunction with TAC to ensure that there will be no detriment to the child’s overall care needs and/or outcomes by discharge).
- When a health professional consider discharge of the child or young person from service because of non-engagement (*Was Not Brought)
- When a professional, external to health has identified, that the child or young person’s needs are not being met.
- Was Not Brought – Children and young people who miss appointments should be coded and recorded in their record as Was Not Brought (Appendix 4)
The RFA form should be completed and submitted to the identified agency /Health service in which the practitioner believes could support child’s unmet needs.
If the practitioner is unsure that the request is appropriate or proportionate -a telephone call to the service to discuss in first instance is recommended. This will allow fuller discussion/ consultation and considerations as well as acceptance and understanding of the case and proposed plan.
In the form a concise summary of any concerns that have been identified as needing addressed by another practitioner, service or agency should be clearly noted
In the event of a Request for Assistance not being accepted due to not meeting service specifications, communication must be established to understand why not and to support/ analyze to next steps.
Escalation will be via Team leader/Lead Nurse/ Service manager to support wider system working to support strategic improved outcomes for children within the requestee service and the requester service. This must be done in a timeous manner to avoid delay to care and interventions to the child and family.
Practitioners involved with the Complex/Vulnerable child should consider the support in line with the GIRFEC 5 key question principals. (Appendix 5 -GIRFEC 5 Questions Practice Checklist.)
This carries an explicit requirement for the Named Person, LHP and TAC to provide assistance by responding as follows:
- Convene a TAC request for assistance where they identify any emerging risks or concerns and feel the current plan is no longer meeting the needs of the child, young person or their family
- Escalate concerns to their line manager where they feel their request for assistance had not elicited the response and support required to address emerging risks and concerns for the child or their family.
- Contribute fully to TAC ,meetings and send a deputy where attendance is not possible
- Ensure they share pertinent information appropriately and timeously with the TAC
- Update child’s healthcare plan to reflect changes.
- Amend frequency of scheduled review meetings as required.
2.7 Evaluation and Review
Children and Young People with exceptional health needs will require ongoing evaluation and review of their health needs.
The membership of the TAC are responsible for these ongoing assessment and review. The membership of the TAC may change in response to the changing needs of the child or young person. If at any time the membership requires to elicit support of specific or specialist service to help assess or meet the needs of the child they should make a RFA to the appropriate professional to elicit this support.
- What is getting in the way of this child’s wellbeing?
- Do we have all the information we need to help this child?
- What can we do now to help this child?
- What can my service do to help this child?
- What additional help, if any, may be needed from others? (Children & Young People Act 2014)
- The predominant needs of the child, young person and family must be met.
- The LHP should have previous or potential relationship with the child or young person.
- The LHP should have an ability to influence and co-coordinate acute, universal and specialist services.
- The LHP and TAC have an understanding of surrounding support systems available to augment universal and specialist services.
- The identified professional has the capacity and capability to work as a Lead Health Professional.
- If the TAC identify group member who feels they do not have capacity to be LHP,the identified person should contact their line manager to discuss this request and how that capacity might be created. – Response to the group with outcome in 48 hours.(With in inpatient services escalation should be to Clinical Director/Lead Nurse and within Health Visiting this would be Team Leader, Senior Nurse or Service Manager).
If a child is in hospital – The LHP should initially be appointed from within the hospital team. It may be appropriate to transfer the LHP role to a community professional as part of discharge planning arrangements
- If Child Protection issues are the predominant needs of the child then a Social Worker will be appointed as the LP. However where the child also has complex health needs – an LHP should also be identified who will coordinate the ‘health’ contribution to interagency child’s plan (The interagency child’s plan remains a single plan and the multidisciplinary healthcare plan becomes a component of this).
- When the child protection issue is addressed it may be appropriate to appoint a different Lead Health Professional. This should be agreed and documented by TAC prior to social work closing the child’s case.
- Where a colleague from education is considered to be the most appropriate person to adopt role of the Lead professional; a Lead Health Professional should continue to be identified for children or young people with complex care needs to ensure that the health contribution to the child’s plan remains coordinated.
- Information should be shared with the Child or Young person’s named person (Health Visitor pre 5 or Head Teacher or Guidance Teacher School age child, in accordance with current guidance on information sharing
There exists a good understanding of what needs to be done to improve outcomes for children and families. GIRFEC wellbeing indicators provide the framework. Local quality assurance and improvement arrangements will provide the evidence and will take a holistic view of systems, alongside service delivery.
Children’s health services will adapt or develop governance arrangements ensuring consistent and robust implementation of the protocol across children’s health services, and which demonstrate a high degree of compliance. Systems and processes will be developed to support ongoing monitoring of the impact of the protocol for children, young people and families/carers.
Those systems and processes will provide ongoing review of set Key Performance Indicators (KPI) and Outcome measures, in line with national outcomes for children and young people as part of the National Practice Framework (NPF).
Universal Pathway HV Antenatal Contact Process (Word document)
The antenatal health visitor contact should be carried out by the Health Visitor between 3234 weeks of pregnancy in line with the Scottish Governments Universal Health Visiting Pathway. This is often the health visitors’ first contact with the family and is crucial for the development of the therapeutic relationship. Research suggests an effective first contact positively impacts on the parents’ use of the service in the long-term.
The antenatal health visitor contact does not replace the care provided by midwifery services. Instead it complements it by working across the antenatal service continuum encompassing hospital, primary care and community services.
The main aims of the contact are to:
Commence a comprehensive and holistic assessment of the expectant mother and fathers’ needs. Giving consideration to mental health and wellbeing of both parents and supporting the transition to parenthood. A variety of health promotion topics including breastfeeding and nutrition, postnatal depression, domestic violence, FGM, safety, smoking cessation and prevention of SIDS will be explored at the contact. The Universal Health Visiting Pathway and local support networks will also be discussed.
The contact will inform the health visitor’s assessment of need for the family at the earliest opportunity and will assist in determining whether the child and their family requires routine universal services or an enhanced health visiting package of care which may include support from partner agencies.
It is important that patients remain confident that their personal information is kept safe and secure. Practitioners must be confident to share information appropriately when protecting vulnerable individuals. Failures of communication lie at the heart of many Significant Case Reviews (SCRs). At the same time, care should be taken to maintain the right to privacy of individuals when it is appropriate to do so.
Professionals should refer to their own professional body’s advice regarding information sharing. For example, the GMC offers this information on Confidentiality and sharing information, the NMC has this Code for nurses and midwives.
The EU’s General Data Protection Regulation (GDPR) came into force in May 2018 and strengthens personal data protection for all individuals within the European Union. New regulations will come into effect to amend the text of the GDPR when the UK leaves the EU. The following are regarded as the ‘seven golden rules’ of information sharing:
- The Data Protection Act 2018 should not be regarded as a barrier to sharing information.
- A record should be kept of what has been shared, with whom and for what purpose, and of every decision made and the reasoning behind it.
- It is important to be open and honest with the individual concerned (and their family, where appropriate) from the outset, about why, what, how and with whom information will, or could, be shared, and to seek their agreement, unless it is unsafe or inappropriate to do so.
- Information sharing should be by consent where appropriate, and, wherever possible, respect the wishes of those who have not consented to share confidential information. Information may be shared without consent if it is believed, based on the facts of the case, that lack of consent can be overridden in the public interest.
- It is important to consider the safety and well-being of the individual concerned, as well as others who may be affected by their actions.
- Information sharing should always be necessary, proportionate, relevant, accurate, timely and secure.
Children and young people who miss appointments should be coded and recorded in their record as ‘Was Not Brought’ (WNB) rather than ‘Did not attend’. This should be clearly documented in EMIS and acute records and form part of the child’s chronology. Consideration should be given to the impact on the health and wellbeing of the child by missing their appointment.
There can be many reasons why they are not presented for their appointment and often isolated missed appointments not a cause for concern. However they can be a sign of neglect or that the family is struggling to meet all appointments if they are multiple. Barriers to attending appointments should be explored including transport and financial challenges.
If child protection concerns are identified staff should follow normal child protection procedures by submitting a notification of concern. This information should be shared with the health LP and allocated SW if already involved.
Children with complex health needs SHOULD NOT be discharged from a service for WNB without discussion with the health LP and a risk assessment undertaken.
Complex Child Protocol EMIS Guidance SOP (pdf)
This Protocol was developed by a multidisciplinary group of professionals working within children’s health services.
The protocol was developed in response to the need to improve and better support children and families navigate often complex patient pathways, and importantly to improve outcomes for those children, by enhancing care coordination and management arrangements.
The protocol adopts GIRFEC (Getting it Right for every Child) practice model, in developing the role of Lead Health Professional (LHP) and TAC (Team Around the Child) and a single health coordination plan.
It sets out clearly the responsibilities of all professionals working in children’s health services in the promotion of team working, information sharing and effective professional to professional communication, in the provision of person centred care. With all adopting a Collaborative communication and coordination ethos.
Complex Child Protocol Coordination Plan SOP (pdf)
In September 2020 the Children’s Health Services Complex Care Management Protocol was ratified by the GGC Child and Maternal Health Strategy Group and the GGC Child protection Forum. It was agreed that to implement this guidance across Children’s Health Services in the board that the oversight would sit with the Getting It Right For Every Child (GIRFEC) Implementation Group.
Four subgroups were agreed to complete work associated with GIRFEC implementation one of which is this group the complex child protocol /Health Lead Professional implementation Group. It should be noted that the production of the Children’s Health services Complex Care Management Protocol was a completed action for a Child Death SCR 2017.
A Health Single agency Child’s Coordination Plan has been developed for all children and young people who meet the criteria within the protocol and have identified Lead Health Professional / involvement of a wider inter/Multidisciplinary Team. This would promote and ensure coordination and communication around admission and discharge of children and young people to improve outcomes. Full implementation of this Plan and required Learnpro module is set for 17th April 2023.
Appendix 10: Complex Care Management Protocol Presentation (2023 v5) (PowerPoint)
This presentation is relevant for all staff working within children's services in NHSGGC.
Last reviewed: 01 March 2023
Next review: 31 March 2025
Author(s): NHSGGC Children’s Health Services
Approved By: Public Protection Forum

