Urticaria not associated with anaphylaxis: management in children
exp date isn't null, but text field is
November 2023: This guidance is currently under review as it has gone beyond the standard review date. It reflects best practice at the time of authorship / last review and remains safe for use. If there are any concerns regarding the content then please consult with senior clinical staff to confirm.
Urticaria refers to erythematous skin lesions, which may be raised (wheals) with flat/macular erythematous edges (flares). The wheal may be white in the centre. Angioedema describes swelling usually, but not always, in combination with urticaria elsewhere. Urticaria is usually immune mediated, but allergy is not the most common cause. Type 1 (IgE mediated) allergy is usually associated with other additional symptoms, such as mouth, tongue or throat itch (if food allergy), swelling, vomiting, breathing difficulty, and rarely, anaphylaxis.
Anaphylaxis is a medical emergency and requires immediate treatment.
|
Symptoms & Signs of Anaphylaxis |
|
Facial/ mouth swelling |
|
Difficulty breathing |
|
Difficulty speaking or swallowing |
|
Feeling of impending doom |
|
Hypotension |
|
Abdominal pain and vomiting |
|
Collapse and unconsciousness |
Urticarial lesions vary in size, are well circumscribed, transient and typically widespread. It is a common presentation to the Emergency Department as it is striking in appearance and often very itchy, causing alarm to parents and discomfort to the child. Urticaria is thought to affect around 20% of the population at some point in their life.
Urticaria can be defined as either acute, lasting less than 6 weeks in duration, or chronic, either lasting longer than 6 weeks or with regular recurrent episodes. Chronic urticaria may be associated with physical stimuli (e.g. dermographism, cold, heat, pressure) and often has an autoimmune component. A detailed history to attempt to identify a trigger, the duration of symptoms, the presence of any facial or mouth swelling, wheezing or difficulty breathing is important.
Triggers for urticaria can include viral illnesses, different allergens and drugs (e.g. penicillin and NSAIDS). In many cases, the trigger is unclear.
Urticaria due to IgE mediated allergy typically occurs within minutes of exposure to the allergen (maximum 1-2 hours) and lasts for a short period (minutes to a few hours).
Urticaria due to viral illness or a drug reaction can last for several hours, days or sometimes weeks. The typical history for urticaria secondary to a viral illness is one where the child has had viral symptoms for a few days prior to the development of an urticarial rash. However, it can appear “out of the blue” with no obvious prodrome.
The rash may come and go over several days, and may not appear to respond to antihistamines. If children wake up at night or first thing in the morning with a widespread urticarial rash, the mechanism is very unlikely to be allergy.
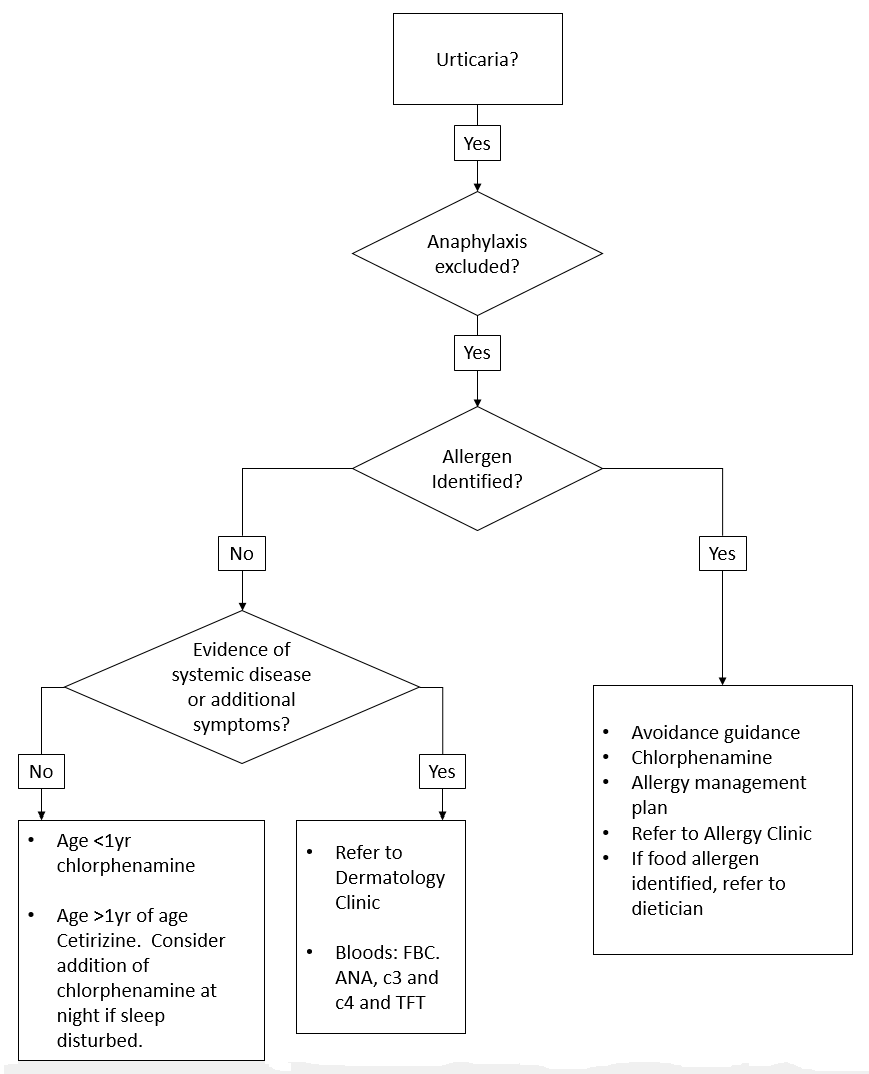
Further investigations are not usually required in the ED, unless there is evidence of systemic disease or additional symptoms such as bruising, which could suggest urticarial vasculitis. If this is suspected, the following investigations should be done in the ED - FBC, ANA, C3 and C4 and TFT - these patients should be referred to dermatology.
- If a specific allergen is suspected, the child should be given chlorphenamine and assessed to ensure they are not developing an anaphylactic reaction. Subsequent avoidance of the potential allergen should be advised. An allergy management plan and chlorphenamine should be given at discharge and the child referred to an allergy clinic. If the history and presentation is diagnostic of a food allergy, then refer to a dietician.
- If no specific trigger is identified, management consists of an antihistamine. If the child is younger than 6 months chlorphenamine should be given. If the child is older than 6 months, a longer acting antihistamine should be used (first line long acting antihistamine is cetirizine).
When to Refer to Dermatology Clinic
Patients should be referred if urticaria persists for longer than 3 months and is unresponsive to 3 successive trials of a long acting antihistamine, each trialled for 4-6 weeks. Children with additional symptoms such as bruising or joint swelling should also be referred to dermatology, as these symptoms may be suggestive of systemic disease. The ED discharge summary can be used to advise the GP on the criteria for referral to a Dermatology Clinic.
Cetirizine Dosage
|
Age |
Cetirizine Dose |
|
1-2 yrs |
250micrograms/kg BD |
|
2-5 yrs |
2.5mg BD |
|
6-11 yrs |
5mg BD |
|
12-18 yrs |
10mg OD |
Chlorphenamine Dosage
|
Age |
Chlorphenamine Dose |
|
1mth-23mth |
1mg BD |
|
2-5 yrs |
1mg every 4-6 hrs (Max 6mg daily) |
|
6-11 yrs |
2mg every 4-6 hrs (Max 12mg daily) |
|
12-18 yrs |
4mg every 4-6 hrs (Max 24mg daily) |
Last reviewed: 11 July 2019
Next review: 31 October 2024
Author(s): Dr Stacey Wightman (Supervisor - Dr Scott Hendry) – Paediatric Emergency Department
Co-Author(s): Consulted with: Dr Rosie Hague - Consultant in paediatric Infectious Diseases / Immunology, Dr Paula Beattie – Paediatric Dermatology Consultant.
Approved By: Paediatric Clinical Effectiveness & Risk Committee
Reviewer Name(s): Steven Foster

