Brief Resolved Unexplained Event or BRUE (ALTE guideline update)
exp date isn't null, but text field is
Objectives
This guideline has been developed for the evaluation, risk stratification, investigation and management of patients presenting to hospital with a brief resolved unexplained event (BRUE). This guideline is intended to replace the previous guidance on Apparent life-threatening events (ALTE), due to updated evidence and reclassification of such presentations.
An ALTE is a descriptive term based on an event that is frightening to the observer including a combination of: apnoea, colour change, change in muscle tone, choking or gagging. This definition includes both physiological and pathological causes for events.
It has been recommended that the term ALTE is replaced with the new term “Brief Resolved Unexplained Event” or BRUE. This concept differs from an ALTE both in definition, and in allowing risk stratification of patients, which in turn can guide further management.
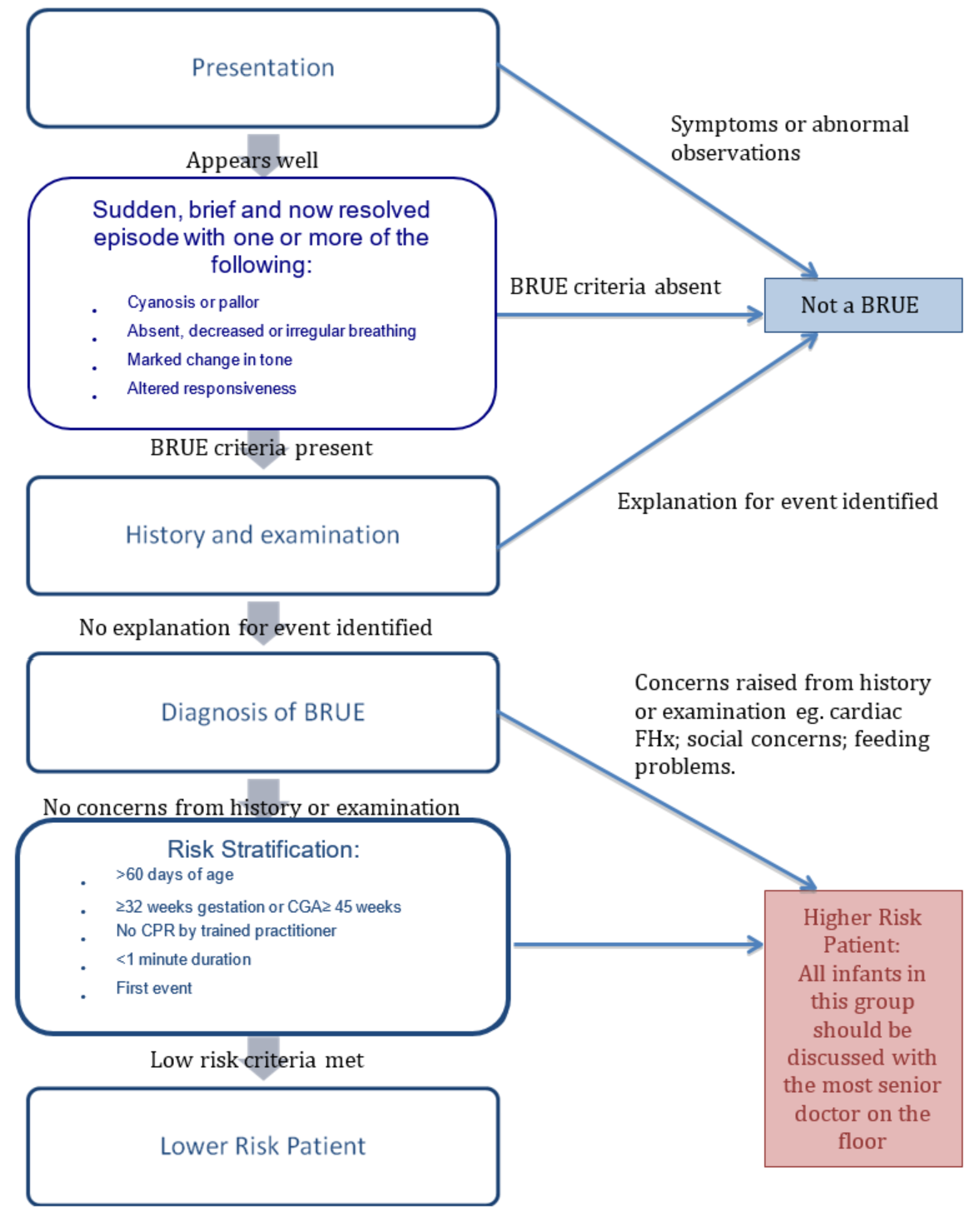
BRUE allows for health care professional to categorise event, and stratify infants as lower or higher risk of having a repeated episode or a serious underlying disorder. Higher risk patients require further investigation +/- treatment.
The diagnosis of a BRUE can only be used as a diagnosis if there is no explanation for the event after a thorough history and examination.
BRUE is defined as an episode in an infant less than 12 months old characterized by:
- < 1 minute duration (typically 20-30s)
- Followed by return to baseline state
- Not explained by identifiable medical conditions
Includes one or more of the following:
- Central cyanosis/pallor
- Absent, decreased or irregular breathing
- Marked change in tone (hyper or hypotonia)
- Altered level of consciousness
 Source: American Academy of Pediatrics; Brief resolved unexplained events (formerly Apparent life-threatening events) and evaluation of lower risk infants. Pediatrics 2016, 137(5): e20160590.
Source: American Academy of Pediatrics; Brief resolved unexplained events (formerly Apparent life-threatening events) and evaluation of lower risk infants. Pediatrics 2016, 137(5): e20160590.
|
Physiological |
Gagging, laryngospasm, neonatal periodic breathing |
|
Cardiac |
Congenital heart disease, arrhythmias, prolonged QT, vascular ring |
|
Respiratory |
Inhaled FB, airway obstruction incl. laryngomalacia, congenital malformation. |
|
Infection |
Pertussis, pneumonia, URTI/LRTI (esp. RSV), meningitis/encephalitis, UTI, septicaemia, gastroenteritis. |
|
CNS |
Head injury, seizures, cerebral malformations, central hypoventilation syndrome. |
|
Non-accidental injury |
Inflicted injury incl. drug ingestion, factitious illness (Munchhausen by proxy), suffocation. |
|
Gastrointestinal |
Gastro-oesophageal reflux |
|
Surgical |
Intussuception, testicular torsion |
|
Metabolic/toxins
|
Hypoglycaemia, hypocalaemia, hypokalaemia, inborn error(s) of metabolism, intentional and non-intentional drug overdose. |
General description of event:
- Who reported/witnessed event?
- Where did it occur?
- What was patient doing immediately before event started?
- Awake or asleep?
- Position: supine / prone / upright/ moving?
- Feeding? How long since last feed? Vomiting or anything near the mouth?
During event:
- Choking or gagging?
- Awake or asleep?
- Moving or quiet?
- Conscious?
- Responsive to voice?
- Muscle tone? Any repetitive movements?
- Distressed?
- Breathing? Struggling to breathe?
- Skin colour: normal/pale/blue/red?
- Colour of lips?
- Bleeding from nose, ears or mouth?
- Eye movements ie. open, closed, blinking, deviated, flickering?
End of event:
- Duration?
- How did it stop: spontaneous/ when picked up / back slaps/ mouth to mouth / chest compressions?
- Sudden or gradual cessation?
- Any treatment given: medications / sugary drink or food?
- 999 called?
After event:
- Back to normal? How long did this take?
- Condition after event: pale / sleepy/ floppy/ poorly responsive/ vomiting etc?
- Anything noticed by parents/carers during period prior to return to baseline? If not returned to normal, what is different?
Recent past medical history:
- Preceeding illness? URTI symptoms / D&V etc.
- Any injuries/falls recently?
Past medical history:
- Perinatal history, including NICU/SCBU admissions.
- Gestational age at birth
- Newborn screening results
- Gastro-oesophageal reflux?
- Breathing patterns eg. snoring, apnoeas.
- Development to date? Meeting milestones?
- Previous unexplained episodes?
- Previous presentations to GP/OOH/ED: illnesses/injuries.
- Any previous resuscitation required? If so, explore the nature of this.
- Any recent hospitalisation/ surgery?
- Recent immunisations an immunisation history? Recent travel?
- Medications: prescribed and over-the-counter.
- Allergies?
Family history:
- Sudden unexplained deaths in 1st/2nd degree relatives under 35; esp. as infant?
- ALTE/BRUE in sibling?
- Long QT syndrome/ arrhythmias?
- Inborn error of metabolism (IEM) or genetic conditions in family?
- Parental consanguinity?
Social & Environmental history:
- Family structure? Who lives at home with child?
- Smokers in house? Drugs or toxic substances at home?
- Anyone unwell at home?
- Any social work involvement with family (both in general; for this patient and for any other siblings in the household?)
- Mental illness or substance abuse at home?
Full ABCDE assessment; with consideration of differential diagnosis.
Observations including temp, RR, HR, BP, AVPU and oxygen saturations.
Plot weight, length and head circumference.
|
Consideration for child protection concerns:
If ANY Child Protection concerns then HIGH RISK and needs to be |
Often after history and examination there may be no specific diagnosis found.
Factors which make the event higher risk:
- Infants < 2 months of age
- History of prematurity esp. if < 32 weeks at birth.
- More than 1 event.
Patients may be classified as lower risk BRUE if they have no concerning feature on history/examination PLUS:
- Age > 60 days
- Born ≥ 32wks gestation and corrected gestational age ≥ 45 weeks
- No CPR by trained health care professional
- 1st event
- < 1 minute total duration
A low risk event is unlikely to represent a severe underlying disorder; and is unlikely to recur. Therefore based on the above risk stratification of patients; it is possible to guide what further investigation of the event, if any, is required.
Please refer to Flow diagram (1) above for guidance
- Lower risk: no investigations required, however capillary blood glucose and urinalysis may be performed if clinical concern.
- Higher risk: discuss with senior doctor (ED Consultant or OOH senior paediatric registrar – phone 84678)
Consider: FBC, UEC, CRP, glucose, naso-pharyngeal aspirate, blood gas, ECG plus any further investigations felt appropriate based on clinical presentation; and referral to relevant guidelines.
By definition if patient requiring ongoing treatment, episode is NOT a BRUE. Lower risk patients do not routinely need admitted for cardio-respiratory monitoring.
Lower risk: Discharge home only if:
- Low clinical suspicion of serious underlying disorder.
- Parents reassured and happy to care for child at home. If not for discussion with medical team for period of inpatient observation.
Provide parents carers with education / advice on BRUE, including worsening statement for representation.
Lower risk does not mean no risk. Lower risk patients could be considered for a period of observation within the ED department if required.
Higher risk: Following discussion with ED Consultant or OOH senior paediatric registrar, consider admission for observation, cardio-respiratory monitoring and further investigations as guided by presentation.
Involve and refer to relevant specialties as appropriate if underlying cause identified:
- Paediatric medicine
- Paediatric general surgery or neurosurgery - Other (e.g. medical or surgical subspecialties)
- Social work/child protection unit if appropriate.
- American Academy of Pediatrics; Brief resolved unexplained events (formerly Apparent life-threatening events) and evaluation of lower risk infants. Pediatrics 2016, 137(5): e20160590.
- Royal Children’s Hospital, Melbourne; Brief resolved unexplained event,
- Dynamed Plus; Brief resolved unexplained event (BRUE),
- Fox, S (2017). Pediatric EM Morsels (CME Website). Published 2nd September 2016; updated 23rd July 2017.
- Tate C, Sunley R. Brief resolved unexplained events (formerly apparent lifethreatening events) and evaluation of lower-risk infants, Archives of Disease in Childhood - Education and Practice; 2017.
Last reviewed: 14 December 2018
Next review: 31 October 2025
Author(s): S Farquharson, S Foster.
Version: 2
Approved By: Paediatric Clinical Effectiveness & Risk Committee

