Hand and finger fractures
exp date isn't null, but text field is
Objectives
Management guidelines for hand and finger fractures in children.
Scope
Children that have sustained hand and finger fractures.
Audience
Emergency Department, orthopaedic and plastic surgery clinicians.
General Principles
Introduction:
- The hand is the most frequently injured body part in children
- The little finger and thumb are the most commonly injured digits
- Crush injuries are the most common injuries in toddlers
- Sporting injuries are the most common in older children
- Most finger fractures if appropriately treated heal without complication
- Complications are often as a result of failure to identify and treat an injury requiring surgery
Clinical Assessment:
- Should record mechanism and site of the injury which is best achieved with a diagram
- Ensure the correct side is identified
- Record hand dominance – which may not be known in young children
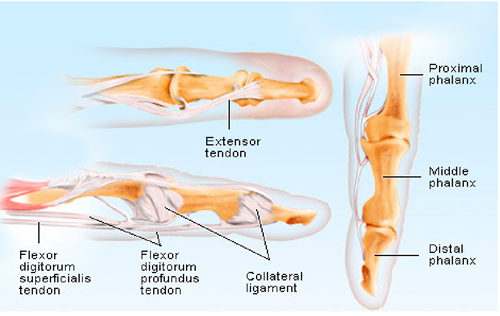
- Stability of appropriate ligaments and relevant tendon function should be assessed
Rotational Deformity:
- This should always be assessed and recorded in finger injuries
- Normally when the fingers are fully flexed they should all point to the scaphoid tubercle
- Ask the child to flex the fingers and observe the planes of the nail beds and look for overlapping or scissoring of the fingers
- In a non-compliant child passive extension of the wrist should flex the fingers
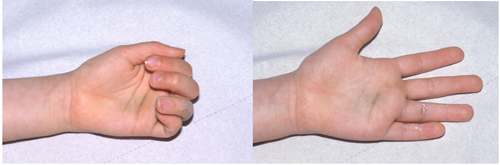
Example of rotational deformity of the ring finger
Imaging
- AP and lateral views of specific individual fingers or the thumb should be requested
- an AP and oblique view of the hand should be requested for metacarpals
Management
- The clinician needs to decide if the fracture is open or closed, un-displaced or displaced and stable or potentially unstable. If there is any doubt, the patient should be discussed with the ED Consultant or Middle grade.
- Neighbour/Buddy strapping is the standard treatment for un-displaced stable finger fractures. The adjacent finger acts as a splint for the injured finger. The tape should avoid the PIP and DIP joints.
- Volar Slabs are used for un-displaced fractures which are potentially unstable. They are applied with the hand in the “position of function” with finger MCP joints flexed and IP joints extended which avoids stiffness. A thumb extension can be added for thumb fractures.
- Patients requiring reduction +/- fixation should be referred to the on-call Plastic Surgery Registrar
Finger Fractures
Phalangeal Fractures
Base Fractures
- Salter Harris type II fractures are the most common and are usually stable fractures
- Un-displaced fractures are treated in buddy strapping.
- Un-displaced fractures can be manged with neighbour strapping and discharged with an advice leaflet.
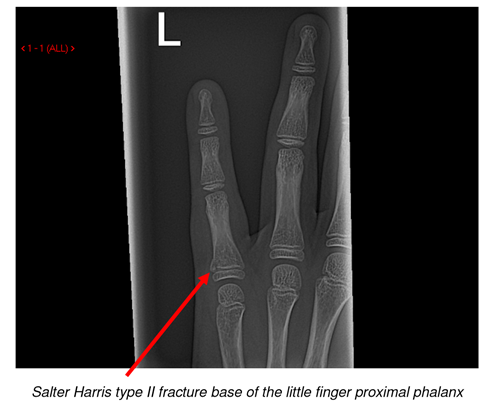
- Displaced fractures should be referred to plastic surgery. They can potentially be reduced using a metacarpal block. Management should be discussed with the on-call plastic surgery registrar. If reduction is performed in ED, the patient should have a check x-ray and be placed in a volar slab. The patient should be referred to the oncall plastic surgery registrar for follow up.
Shaft Fractures
- Buckle or torus fractures are stable. They can be treated with neighbour strapping for 1 week
- Discharge with advice leaflet
- Displaced fractures should be referred to the on call plastic surgery registrar.
- Un-displaced spiral or oblique fractures are potentially unstable and prone to rotation. Rotational deformity must be carefully assessed. These fractures should be treated in a volar slab and the patient referred to the on-call plastic surgery registrar for follow up.
- Transverse fractures are usually stable and can be treated with neighbour strapping and referred to the on-call plastic surgery registrar for follow up.


Neck / Peri-articular fractures and Intra-articular fractures
- These are complex fractures prone to instability and should be referred to the on-call plastic surgery registrar at the time of presentation.


Volar Plate Injuries
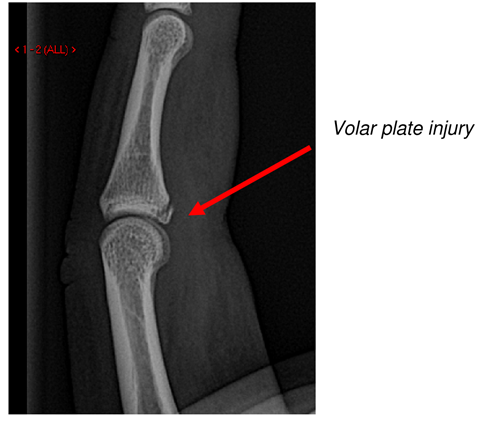
- A hyperextension injury causes an avulsion flake fracture from the volar surface of the base of the middle phalanx
- Clinically the finger will have a fusiform swelling around the PIP joint
- Check for stability, as severe volar plate injuries where there is instability in a dorsal direction should be treated in extension block splint with mobilisation in flexion for 4 weeks. These patients should be referred to the plastic surgery registrar on call.
- Flake fractures can be treated with neighbour strapping for 1 week followed by mobilisation
- These injuries do not require follow up but patients should be advised pain and swelling is likely to persist for several weeks. Discharge with advice leaflet.
Central Slip Avulsion fracture
- This is an avulsion fracture from the dorsal surface of the base of the middle phalanx
- This needs to be treated with splinting in a volar slab and referred to the on-call plastic surgery registrar for follow up.
Mallet Fingers
- These occur often after minor trauma when the extensor tendon is avulsed from the base of the distal phalanx with or without a bony fragment.
- The distal phalanx droops down when the patient holds their fingers in extension
- These injuries are treated in a Mallet splint for 8 weeks.
- Specific guidance should be given to patients/parents regarding the care of their finger in a Mallet splint. Discharge with advice leaflet
- Caution: Mallet Avulsion fractures where there is displacement of a substantial amount of joint surface involved (approx. > 25 % of the surface), should be referred to the plastic surgery registrar on-call for consideration of fixation.

Mallet Splint
Distal Tuft Fracture
- Closed:are usually caused by a crush injury, are stable fractures which can be treated with neighbour strapping and require no follow up
- Open: these fractures usually have an associated nail bed laceration
- Significant lacerations or injuries with any evidence of deformity or rotation of the finger tip should be referred to the on call plastic registrar for review and possible closure in theatre
Thumb Fractures
- Fractures of the phalanges should be managed in a similar way to finger fractures.
- A wrist splint with a thumb extension should be used instead of buddy strapping. If the fracture requires immobilisation they should be managed in a volar slab with a thumb extension

Example of displaced Salter Harris II fracture of the base of the thumb proximal phalanx
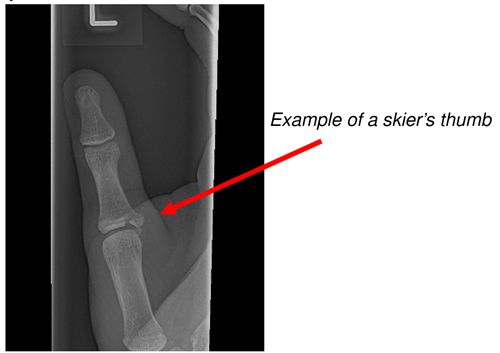
Skiers Thumb
- This injury is caused by forced abduction of the thumb
- These are Salter Harris III intra-articular fractures that avulse the ulnar collateral ligament insertion at the base of the thumb proximal phalanx. The MCP joint will be unstable
- These patients should be referred to the oncall plastic surgery registar as some patients may require surgery
Metacarpal Fractures
Little finger Metacarpals
- Fractures of the neck of the metacarpals can be treated conservatively with neighbour strapping and do not require follow up. Discharge with advice leaflet.
- BEWARE of fractures with associated teeth marks or lacerations from punch injuries. These patients should be referred to the plastic surgery registrar to be washed out in theatre.
- Fractures of the base of the little metacarpal should also have an Xray true lateral view of the hand to ensure there is no dorsal displacement. The patient should be managed in a volar slab and referred to the on-call plastic surgery registrar for follow up.
Metacarpal shaft fractures
- Spiral fractures should be carefully assessed for rotational deformity, and if present should be referred to the plastic surgery registrar on call.
- Otherwise these fractures are generally stable and can be managed with neighbour strapping and discharged with an advice leaflet.
Base of Thumb Metacarpal Fractures or Bennet’s fracture
- Un-displaced fractures can be treated in a volar slab with a thumb extension or a Bennet’s cast if there is no swelling and staff available to apply this cast. Follow up at orthopaedic fracture clinic.
- Displaced fractures should be referred to the on-call orthopaedic surgeon.
Editorial Information
Last reviewed: 11 July 2016
Next review: 31 October 2025
Author(s): Dr Fiona Russell
Approved By: Clinical Effectiveness

