RHCG Major Trauma Team Emergency Department Activation and Response - Standard Operating Procedure
exp date isn't null, but text field is
Objectives
- To outline the criteria for triggering a Paediatric Major Trauma Team response
- To outline a standardised procedure for activating a Paediatric Major Trauma Team response
- Defining the roles and responsibilities of the Paediatric Major Trauma Team
- Defining ‘trauma call’ and ‘trauma pause’
Scope
This document applies to patients under 16 who are suspected to have sustained major trauma.
Audience
Paediatric Emergency Department clinicians and specialty teams with a remit for trauma.
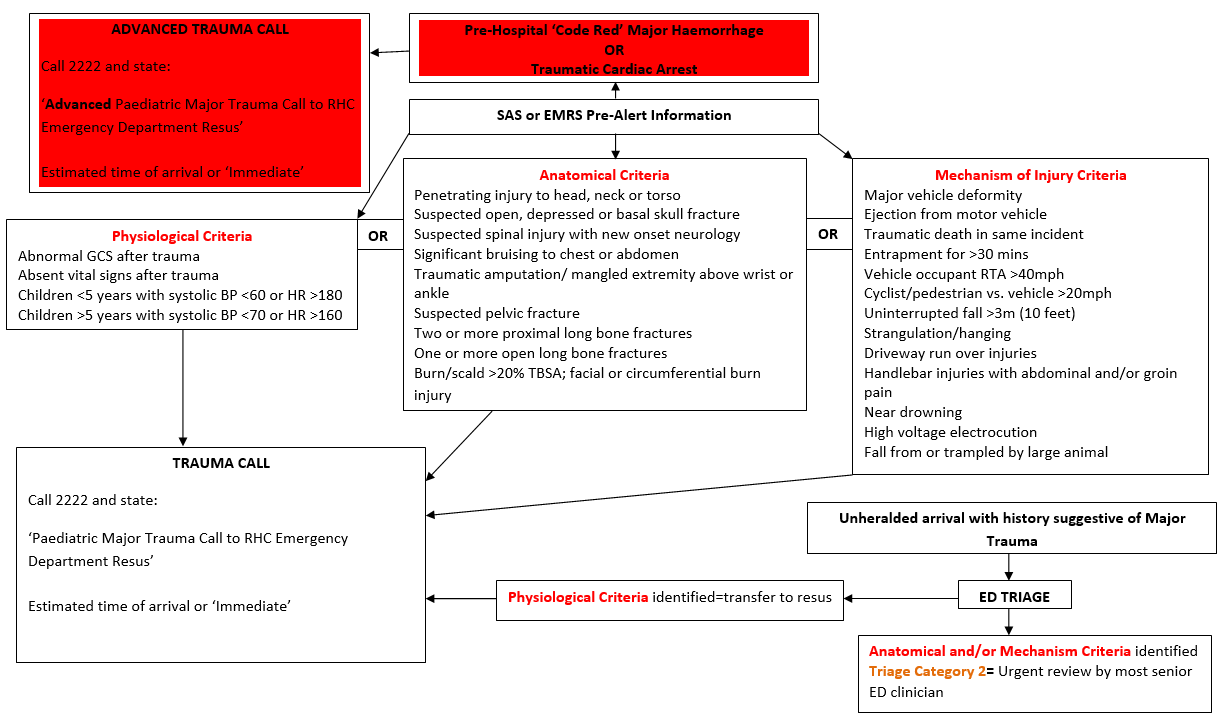
Physiological criteria
- Abnormal GCS after trauma
- Absent vital signs after trauma
- Children <5 years with systolic BP <60 or HR >180
- Children >5 years with systolic BP <70 or HR >160
OR
Anatomical criteria
- Penetrating injury to head, neck or torso
- Suspected open, depressed or basal skull fracture
- Suspected spinal injury with new onset neurology
- Significant bruising to chest or abdomen
- Traumatic amputation/ mangled extremity above wrist or ankle
- Suspected pelvic fracture
- Two or more proximal long bone fractures
- One or more open long bone fractures
- Burn/scald >20% TBSA; facial or circumferential burn injury
OR
Mechanism of Injury Criteria
- Major vehicle deformity
- Ejection from motor vehicle
- Traumatic death in same incident
- Entrapment for >30 mins
- Vehicle occupant RTA >40mph
- Cyclist/pedestrian vs. vehicle >20mph
- Uninterrupted fall >3m (10 feet)
- Strangulation/hanging
- Driveway run over injuries
- Handlebar injuries with abdominal and/or groin pain
- Near drowning
- High voltage electrocution
- Fall from or trampled by large animal
If none of the above criteria are met but there is clinical concern a trauma call should be initiated at the discretion of most senior ED clinician
For patients that arrive unheralded with a history suggestive of major trauma, an assessment of the above criteria will be made at triage with one of the following outcomes:
- If an anatomical and/or mechanism trigger is identified the patient will be assigned a triage category 2 and an urgent review undertaken by the most senior ED clinician. If required a trauma call can be initiated following that review.
- If a physiological trigger is identified, either in isolation or in addition to an anatomical and/or mechanism trigger the child will be taken into resus and a trauma call initiated from triage (via the ED co-ordinator and senior ED clinician.)
The minimum ED response to a trauma call, irrespective of time of day, will consist of:
- ED consultant (to be called in if off site at time of pre-alert)
- ED middle grade doctor
- ED junior doctor
- X4 ED RNs
- X1 ED HCSW
The formal trauma team call out list held by RHCG switchboard is as follows:
|
Tier 1 |
Tier 2 |
|
ED Consultant/Registrar |
ED Consultant if not already present |
|
PICU Fellow |
PICU Consultant |
|
PICU Nurse |
Anaesthetic Consultant |
|
Anaesthetic Registrar |
General Surgical Consultant |
|
Airway Assistant |
Neurosurgical Consultant |
|
General Surgical Core Trainee/Registrar |
Cardiothoracic Consultant |
|
Orthopaedic Registrar/Consultant |
Radiology Consultant |
|
Hospital Cover |
|
|
Trauma Porter |
|
|
Duty Radiographer- will contact CT radiographer if CT likely from pre-alert details |
|
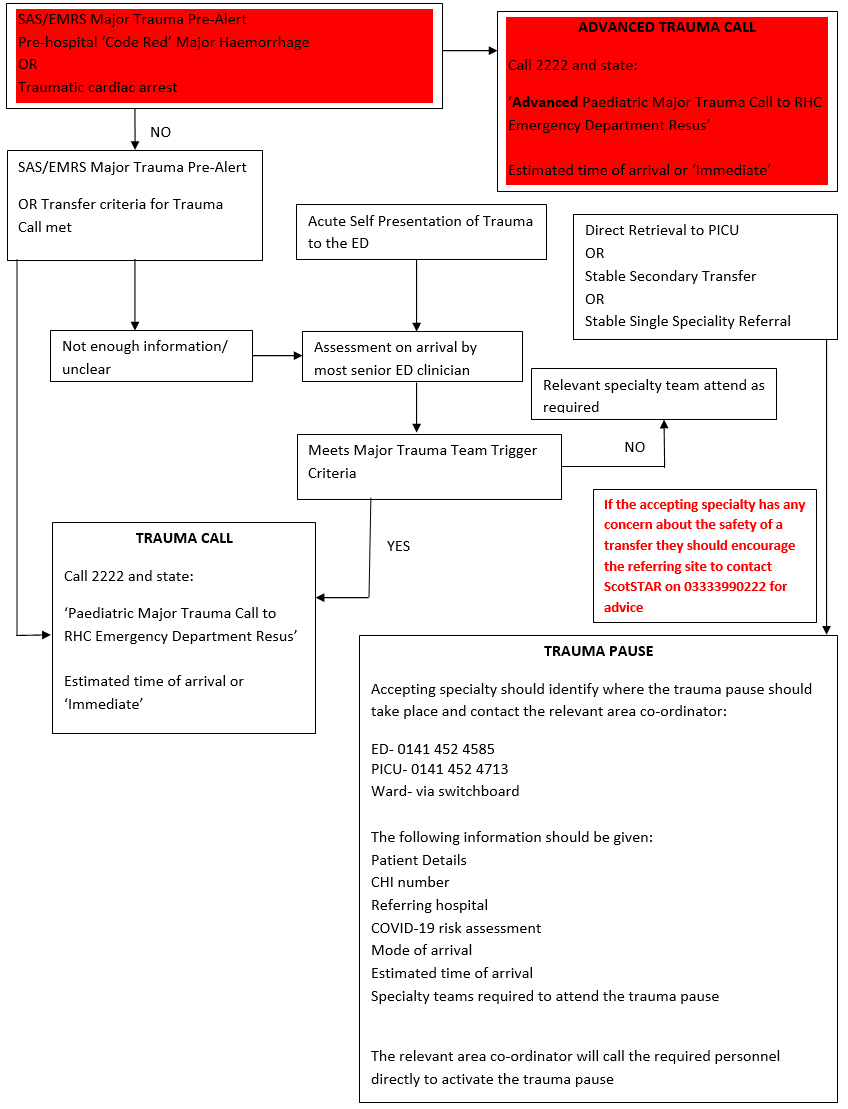
The Paediatric Major Trauma Team can be activated in 3 ways:
Trauma Call
A trauma call should only take place in the ED and can be initiated by ED staff in the following circumstances:
- Any of the above triggers are deemed to be met from a pre-alert call to RHC-G from SAS/EMRS
- Any of the above triggers are deemed to be met for an unheralded/‘walk in’ case to RHC-G AND a trauma call is deemed necessary following review by the most senior ED clinician.
- A modified primary transfer undertaken by ScotSTAR
- Any secondary transfer from another ED where there is:
- Physiological instability
- Diagnostic uncertainty
- Specific intervention required e.g. CT imaging/ preparation for theatre
- Polytrauma where clinical ownership is unclear
- Unexpected clinical deterioration en route to RHCG (this should be called ahead to ED to allow reception in resus)
- Time critical transfer undertaken by the referring site (provided that this does not delay time to definitive care e.g. neurosurgery)
When indicated a trauma call should be initiated through switchboard on 2222. The following information should be given:
1) ‘Paediatric Major Trauma Call to RHC Emergency Department Resus’
2) Estimated time of arrival or ‘Immediate’
A response is expected from ALL Tier 1 and relevant Tier 2 members.
Once a trauma call has been initiated, the ED resus greeter role should be established and trauma team members should be briefed and directed to the appropriate resus space on their arrival in ED.
Advanced Trauma Call
An advanced trauma call triggers the immediate call out of the tier 2 duty consultants by the tier 1 responders. It is a rare event, reserved for a very specific set of circumstances where the junior tier 1 response is thought to require immediate consultant support, irrespective of the time of day. This should only take place in ED and should be activated in the following circumstances only:
- Pre-hospital ‘Code Red’ activation of the Major Haemorrhage protocol for trauma
- Traumatic cardiac arrest
When indicated an advanced trauma call should be initiated through switchboard on 2222. The following information should be given:
1) ‘Paediatric Advanced Major Trauma Call to RHC Emergency Department Resus’
2) Estimated time of arrival or ‘Immediate’
In the context of life threatening haemorrhage and/ or prehospital administration of blood products a ‘Code Red’ activation of the Major Haemorrhage Protocol should also be done via 2222.
On receipt of an advanced trauma call, all tier 1 responders will contact their respective on call consultants (tier 2) as their first action, and ask them to attend RHCG ED resus. Tier 1 responders will then proceed to ED for a briefing.
This will mobilise the following on call consultants:
- Emergency Medicine (if not already on site)
- PICU
- Anaesthetic
- General Surgical (may choose to also call ECLS consultant if required)
- CT Radiographer- called by on site radiographer (discussion with duty radiologist still required)
In addition- the duty theatre manager will stop theatre where possible and ensure the emergency theatre team are called out and that the level 1 fluid warmer and emergency trauma theatre trolleys are taken to ED resus.
Any additional on call consultants required for an advanced trauma call will be contacted by a nominated member of ED staff in the following circumstances:
- Penetrating chest/neck trauma associated with deranged physiology, code red major haemorrhage or cardiac arrest:
Cardiothoracic consultant (this will trigger a separate theatre SOP to mobilise cardiac theatre and perfusion teams)
- Significant head trauma:
Neurosurgical consultant
Trauma Pause
A trauma pause allows a multidisciplinary review of a non-time critical patient arriving at RHC-G for definitive/specialist trauma care following initial assessment and management elsewhere (most commonly another ED). A trauma pause does not always need to take place in the ED. It can take place in PICU or in a ward area, depending on the condition of the patient, and is the responsibility of the accepting specialty to coordinate.
A trauma pause is indicated in the following circumstances:
- Ventilated, stable patient being escorted by the paediatric retrieval service directly to PICU (the trauma pause can be undertaken on arrival to PICU)
- Stable secondary transfer requiring MTC level care
- Tertiary referral requiring specialist input only available at the paediatric MTC
- Apparently stable single specialty injuries
Note patients being transferred to RHCG for specialist care from an inpatient bed elsewhere should not be transferred until an appropriate inpatient bed is identified for them at RHCG. They should proceed directly to that bed on arrival to RHCG and do not require a trauma pause or to be seen in the ED.
If a trauma pause is deemed necessary the accepting clinician should contact manager of the relevant clinical area where it will take place to organise this. For ED this will be the shift co-ordinator on 0141 452 4585. For PICU this will be 0141 452 4713. The following information should be given:
- Patient Details
- CHI number
- Referring hospital
- COVID-19 risk assessment (where appropriate)
- Mode of arrival
- Estimated time of arrival
- Specialty teams required to attend the trauma pause
- Accepting specialties are requested to encourage referring sites to contact the ED/ PICU co-ordinator when the patient is leaving.
A response is required from a selected group of Tier 1 and Tier 2 members, depending on the nature of injuries and at the discretion of the accepting team. Required clinicians will be contacted directly by the relevant area manager/co-ordinator and asked to attend the trauma pause.
Last reviewed: 19 October 2023
Next review: 31 October 2025
Author(s): Dr. Marie Spiers & Dr Christina Harry (Joint RHC Clinical Leads for Trauma)
Co-Author(s): Dr Mark Davidson (Consultant in Paediatric Intensive Care), Dr Vince Choudhery (Consultant in Paediatric Emergency Medicine)
Approved By: Joint Clinical Leads for Trauma, RHC