Trauma team roles and responsibilities
exp date isn't null, but text field is
November 2023: This guidance is currently under review as it has gone beyond the standard review date. It reflects best practice at the time of authorship / last review and remains safe for use. If there are any concerns regarding the content then please consult with senior clinical staff to confirm.
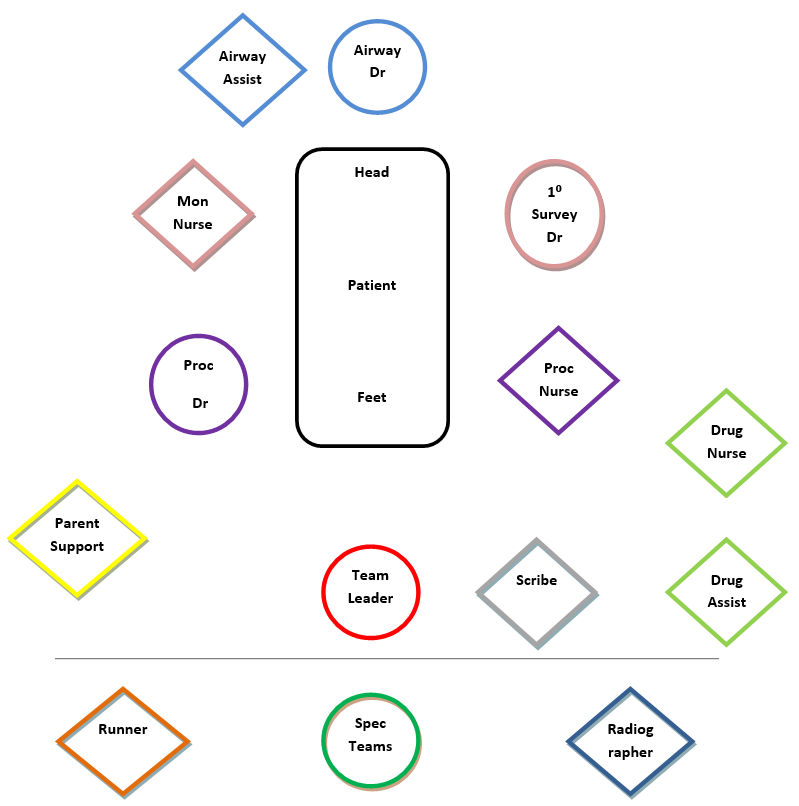
The trauma team is a multidisplinary team of individuals taken from relevant specialties across the hospital that work together to assess and manage children that have sustained traumatic injuries. Their actions are co-ordinated by a team leader.
The primary aim of the trauma team at RHC is to rapidly assess, resuscitate and stabilise the paediatric trauma patient, identify the extent of the injuries sustained and prepare them for early definitive care.
The trauma team structure will vary according to a number of factors which include time of day, availability of staff, skill set of responders and hospital resources. Clearly allocated roles and responsibilities are essential to the effective functioning of the trauma team. This document sets out the recommended ‘default’ allocation of roles. However, it is important to recognise that the assignment of roles should be flexible and focus on optimising the capabilities of its members based on the resources available at any given time.
Default allocation: ED consultant
Other suitable allocations: ED registrar
- Must be clearly identifiable in this role, hands off and stands at the foot of the bed.
- Takes overall control of the trauma resuscitation, makes critical decisions and prioritises care.
- Ensures trauma call is appropriately activated.
- Performs pre-arrival team briefing and role allocation.
- Ensures adequate PPE worn by all key personnel.
- Establishes consistent communication between members with all instructions and feedback going through team leader.
- Co-ordinates handover from pre-hospital colleagues (controlled quiet hands off handover).
- Determines expected need for CT imaging and facilitates communication with CT radiographer/ radiologist.
- Ensures safe, timely and thorough assessment of the trauma patient and ensures all key personnel are aware of the priorities of care.
- Performs a formal handover to the appropriate specialist team for definitive care and ensures the role of team leader is formally handed over.
- Ensures adequate contemporaneous notes are completed and scanned onto Portal prior to the patient leaving the ED (where possible).
- Co-ordinates and leads a ‘hot’ debrief.
The person present at the trauma call with the most airway management experience should fulfil this role.
Default allocation: Anaesthetic consultant
Other suitable allocations: PICU consultant/ registrar or anaesthetic registrar
- Ensures adequate PPE is worn.
- Ensures preparation of required airway equipment.
- Communicates the desired intubation and emergency drugs to the drugs nurse.
- Check and set up ventilator.
- Responsible for assessment and management of airway and ventilation.
- Ensures cervical spine immobilisation at all times.
- Communicates airway assessment to team leader.
- Performs intubation if required ensuring use of the intubation checklist.
- Establishes patient on ventilator.
- Controls 20° tilt to allow assessment of the back of the patient.
- Ensures adequate sedation and muscle relaxation.
- Responsible for the care of the trauma patient on transfer within the hospital (i.e. CT, theatre, PICU).
- Ensures contemporaneous documentation of airway assessment and management in the patient’s notes prior to the patient leaving the ED where possible.
Default allocation: Theatre ODA/ anaesthetic nurse
Other suitable allocations: Anaesthetic trainee
- Ensures adequate PPE is worn.
- Assists airway doctor in preparing for airway intervention.
- Assists airway doctor with interventions.
- Accompanies trauma patient on transfer within the hospital.
Default allocation: ED registrar
Other suitable allocations: ED junior doctor, PICU fellow, surgical registrar/ junior
- Ensures adequate PPE is worn.
- Completes ‘WETFLAG’ calculations prior to patient arrival based on estimated weight.
- Ensures vac mat on trolley before arrival +/- any relevant kit i.e. limb splint, pelvic binder etc.
- Undertakes the primary survey.
- Communicates vital signs and relevant positive and negative findings from primary survey to the trauma team leader and scribe.
- Takes ‘AMPLE’ history from patient +/- parents, communicates this to trauma team leader and documents history clearly in resus notes.
- Requests relevant imaging after discussion with trauma team leader.
- Where appropriate undertakes secondary survey.
- Documents primary +/- secondary survey findings clearly in resus notes and highlights tasks that still need to be completed.
- Ensures all drugs and fluids are appropriately prescribed and signed for.
- Ensures the patient is kept warm.
Default allocation: ED registrar/ junior doctor
Other suitable allocations: PICU fellow, surgical registrar/ junior
- Ensures adequate PPE is worn.
- Prepares IV and IO access equipment (including rapid infuser).
- Gains IV or IO access and takes blood samples.
- Ensures bloods have been sent and utilises Trackcare paediatric trauma order sets.
- Communicates the results of any POCT to the trauma team leader.
- Liaises with blood bank regarding the need of any blood/ blood products.
- Ensures any blood/ blood products are appropriately prescribed, checked and signed for.
- Administers tranexamic acid if indicated and not already given.
- Applies pelvic binder if indicated and not already done.
- Performs chest decompression/ chest drain insertion if appropriate.
- Performs CPR if required.
- Ensures early provision of appropriate analgesia.
- Assists with 20⁰ tilt.
- Performs FAST scan if adequately trained and clinically appropriate (will be determined by the team leader.)
- Assembles kit required for transfer.
Default allocation: ED nurse
- Assembles all resus documentation prior to patient arrival.
- Documents trauma team members including arrival time and role allocation.
- Ensures stop clock is activated on arrival of patient.
- Responsible for accurately recording timeline of events and interventions throughout the resuscitation.
- Records drug doses, timing and route of administration.
- Responsible for documentation of contemporaneous vital signs, including GCS, and completion of a PEWS score.
- Communicates any identified trends in physiology to the team leader.
- Documents salient findings from primary survey.
- Documents transfer time and location.
- Responsible for gathering and documenting any patient belongings, including packing into evidence bags where necessary.
Default allocation: ED nurse
Other suitable allocations: PICU nurse
- Ensures adequate PPE is worn.
- Cuts and removes clothing where required.
- Attaches monitoring equipment to patient including 3 lead ECG, appropriately sized BP cuff, SpO2 and defib pads if required.
- Ensures appropriate tone and cycling time on monitor.
- Takes temperature using appropriate method (including low reading rectal probe if needed.)
- Communicates vital signs clearly to team leader and scribe.
- Ensures name band is applied to the patient.
- Size and insert NG tube if requested by team leader.
- Ensures appropriate collection of urine when possible in the non catheterised patient.
- Sets up external warming blanket and ensures the patient remains normothermic throughout the resuscitation unless otherwise instructed by the team leader.
Default allocation: Senior ED nurse
Other suitable allocations: PICU nurse
- Must be clearly identifiable in this role and delineated by wearing a purple apron.
- Must not be tasked with any other responsibilities and must not be interrupted whilst drawing up drugs.
- Prepares a blank drug Kardex ahead of patient arrival.
- Prepares fluid boluses according to estimated weight ahead of patient arrival.
- Prepares drugs as requested throughout resuscitation including RSI agents, emergency drugs, analgesia and antibiotics using resus guidelines and monographs.
- Prepares infusions and boluses for sedation as instructed.
- Checks all drugs, fluids and infusions with a second staff member.
- Ensures all drugs, fluids and infusions are adequately labelled, prescribed and signed for.
- Ensures the details of all drugs, fluids and infusions made up are clearly communicated to the administering clinician and are signed for as given.
- Ensures CD records are updated, accurate and signed.
- Prepares and packages any drugs for transfer as instructed.
Default allocation: ED nurse
Other suitable allocations: PICU nurse, ENP
- Ensures adequate PPE is worn.
- Assists procedure doctor with preparation of IV/ IO access equipment and fluid warmer.
- Sets up for advanced procedures as directed by the team leader including arterial and central lines, chest drains and urinary catheters.
- Assists with any required advanced procedures.
- Assists with administration of fluid boluses and or drugs.
- Assists with 20⁰ tilt.
- Performs CPR if required.
- Primary role of managing blood product transfusions where required, including appropriate checking of blood products and ensuring they are appropriately prescribed and signed for.
- Assists procedure doctor in preparing for transfer.
Default allocation: ED health care assistant
- Ensures adequate PPE is worn.
- Directs trauma team member to correct resus bay.
- Responsible for processing POC blood gas and returning result to team leader.
- Responsible for organising blood tests to be relayed to labs.
- Responsible for obtaining O Neg blood from theatre stock as directed by team leader.
- Responsible for collecting blood products from blood bank as directed by team leader.
- Responsible for collecting any required kit from other areas e.g. theatres or PICU.
Default allocation: ED health care assistant
Other suitable allocations: ED nurse, ED junior doctor, ENP.
- Greets the family on arrival and stays with them throughout the resuscitation either within the resus room or in the relative’s room as per the parent/ carer’s wishes.
- Identifies key personnel to the family.
- Updates the family with general information regarding their child’s care.
- Communicates any key information from the family to the team leader.
- Assists the family with contacting any other relatives or required support e.g. chaplain.
- Provide refreshments where needed.
- Remain with the family during any updates from medical staff.
- In the event of the child dying the staff member will remain with the family when they are informed of the death and for the remainder of their time in the ED.
- Ensures key personnel are wearing lead aprons.
- Performs any imaging required from primary survey and ensures they are appropriately requested.
- Performs any secondary survey imaging as required.
- Liaises with on call CT radiographer to provide timely availability of CT if required following discussion with the team leader.
Specialty teams will assist with secondary survey and any advanced procedures as directed by the team leader and provide expertise in their specialist area. Second tier teams will be contacted individually, depending on the injury pattern sustained at the request of the team leader.
Last reviewed: 19 October 2023
Next review: 31 October 2024
Author(s): Dr Marie Spiers
Approved By: ED Guidelines Group

