Blind broncho-alveolar lavage (Blind BAL) (PICU)
Objectives
The purpose of this guideline is to establish clear guidance on how to perform a blind bronchoalveolar lavage (Blind BAL).
Scope
This guideline should be followed by any healthcare professional involved in performing a BBAL in the paediatric intensive care setting.
Audience
All staff involved in performing a Blind BAL should be aware of this guideline and be trained and competent to carry the procedure if performing a Blind BAL.
Blind bronchoalveolar lavage (BBAL) is an invasive method of obtaining a microbiological sample from the lower airways. It can be used to aid the diagnosis and antibiotic management of a suspected lower respiratory tract infection or a ventilator associated pneumonia (VAP). Studies have shown that the diagnostic yield from Blind BAL is comparable to direct/bronchoscopically guided BAL[i]. The sensitivity of Blind BAL has been reported as 96%, specificity of 80%, positive predictive value of 88%, negative predictive value of 92% and accuracy of 90% when the cut-off of ≥103cfu/ml was used[ii].
Indications for Blind BAL:
- Part of a septic work-up of a ventilated patient.
- Always consider after intubation or re-intubation
- Clinical or radiological suspicion of pneumonia
- Intubated bronchiolitis patient
Contra-indications to a Blind BALii
- Severe bronchospasm
- Cardiopulmonary instability
- Severe hypoxia
- Use with caution if pulmonary hypertension exists: pre-medicate with fentanyl (1-2mcg/kg)
- Pulmonary haemorrhage in the last 24 hours
- Severe coagulopathy
Complications of a Blind BAL:
- Desaturation – therefore pre-oxygenation for 2 minutes is undertaken except if the patient has a balanced cardiac physiology
- Vagal stimulation and secondary reduction in heart rate
A Blind BAL can be undertake between 0400Hrs and 2000Hrs only and should be dispatched to the labs between 0800Hrs and 2000Hrs seven days a week as they will not be analysed out with this time period. Specimens undergoing a prolonged period of storage prior to examination decrease show a reduced yield. The sample will need to be analysed within 12 hours of collection. If the sample is taken overnight please store in the PICU “lab fridge” for routine morning sample pick-up or send to Microbiology from 0800Hrs in the pneumatic tube system.
|
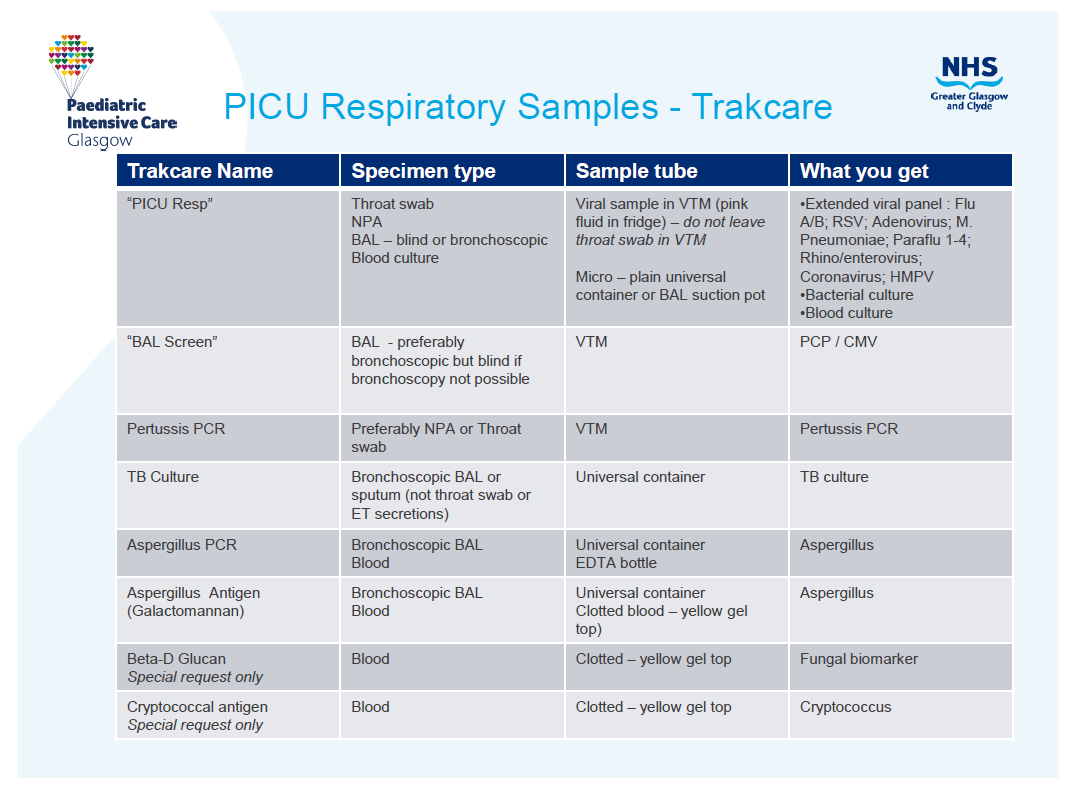
Blind BAL equipment - see picture 1. (all stocked in labelled tray in PICU store room) |
|
1 Sterile drape |
|
2 Sterile gloves & plastic apron |
|
3 Two tracheal suction traps (Ref 24006182) |
|
4 10ml syringe |
|
5 Normal saline |
|
6 Sterile green needle |
|
7 3-way tap (Ref 876.20) |
|
8 Male-male connector (Ref 893.00) |
|
9 Luer lock suction connector (Ref 801.00) |
|
10 Argyle suction catheter 6, 8 or 10Fr gauge (use the largest size that will fit the ET Tube) |
|
11 Blind BAL trolley |
|
12 Spare suction catheter for after Blind BAL |
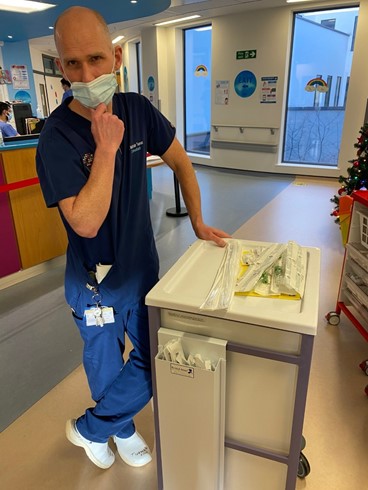
Picture 1: Blind BAL trolley
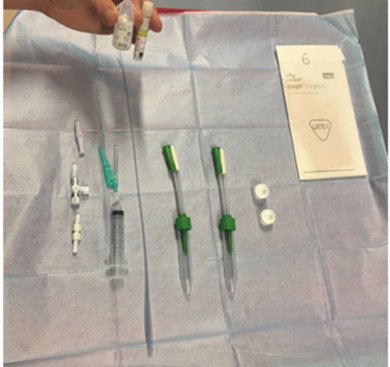
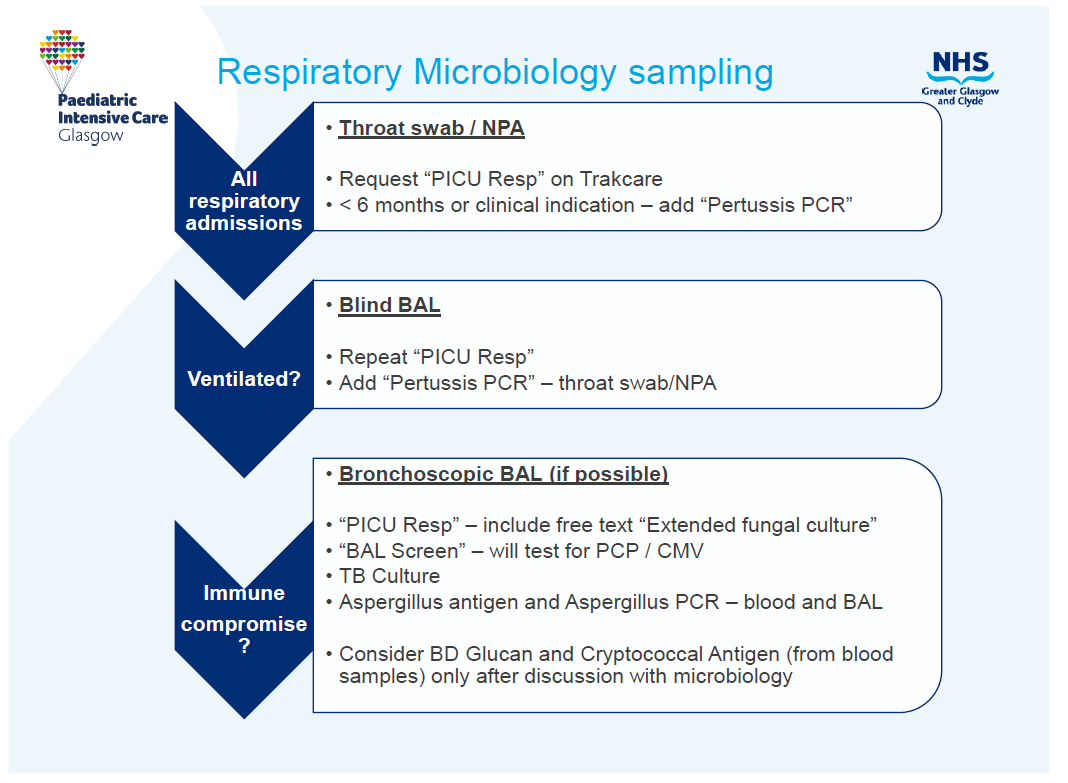
Picture 2: Blind BAL equipment laid out on trolley
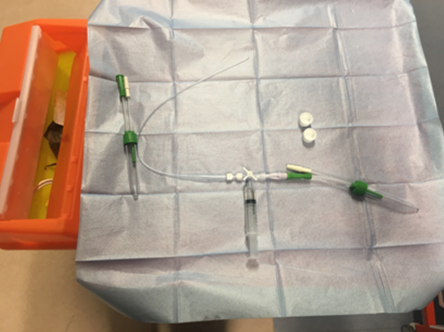
Picture 3: Equipment assembled
|
Action |
Rationale |
|
At the bedspace prepare the sterile field on top of the cleaned Blind BAL trolley:
|
There is a risk of introducing infection if asepsis is not maintained. |
|
Draw up saline using the green needle with an air “chaser” to flush in saline:
|
The “air chaser” is required to flush in all the saline |
|
Assemble the Blind BAL equipment (picture 2 & 3):
|
It is important not to suction tracheal secretions from the ETT while performing BBAL. This would make the interpretation of the result difficult. |
|
Give sedation (if required) and pre-oxygenate for 2 minutes (unless balanced cardiac physiology) |
Pre-oxygenation is mandatory for all patients except balanced cardiac conditions |
|
Advance the Argyle suction Blind BAL catheter gently until resistance is met ensuring that it is advanced beyond the length of the ETT |
This will mean Catheter is normally wedged down right main stem bronchus. |
|
Inject the saline with the syringe held vertically down the ETT so the air “chaser” is last down the ETT |
|
|
Keep the Argyle suction catheter in the same position and open the three-way tap to the suction & suction for 2-4 seconds pulling the Blind BAL catheter up a maximum of 2cm |
|
|
After the sample has been collected, close the three-way tap to suction to ensure that no tracheal secretions are collected and pull out the Argyle catheter |
|
|
Do not aspirate through the catheter once the catheter has been removed from the ETT. Routine ETT suction may be needed after a Blind BAL is undertaken |
|
|
If enough sample decant half the sample into a 2nd plain container and send this to Virology for extended respiratory virus PCR. If not enough sample then repeat the process using a clean argyle suction catheter to get the sample for Virology |
|
|
Order investigations as per trakcare plan – see below the label & send to the microbiology or virology lab:
|
We do not now routinely gram stain Blind BAL’s or perform TB culture The sample will need to be analysed within 8 hours of collection or 12 hrs if sample taken overnight and stored in fridge |
|
Document event on CIS under “event” as Blind BAL |
|
i. Valencia M, Torres A. Ventilator‐associated pneumonia. Current Opinion in Critical Care. 2009;15:30‐35
ii. Sachev A, Chugh K, Sethi M, et al. Diagnosis of ventilator‐associated pneumonia in children in resource‐limited setting: A comparative study of bronchoscopic and non‐bronchoscopic methods. Pediatr Crit Care Med. 2010;11(2):1‐9
Last reviewed: 01 December 2021
Next review: 31 December 2024
Author(s): I McLeod, J Ballard, K Harvey Wood, M Harvey, N Spenceley, M Davidson
Version: 5.1
Approved By: PICU Guideline Group