Endotracheal tubes, cuffed
exp date isn't null, but text field is
Objectives
- To allow standardized use of all cuffed ETT’s in PICU and to facilitate the education of all staff groups.
- Minimise the potential for subglottic injury secondary to inadvertent high cuff pressures or inadvertent oversized uncuffed ETT’s being sited.
- Enable routine documentation of cuff pressures in all patients with cuffed ETT’s in place and allow us to audit and monitor our adverse events and outcomes.
Scope
This guideline applies to any patient being ventilated via a cuffed ETT in PICU.
Audience
All healthcare professionals in paediatric critical care involved in the care of ventilated children should be familiar with this guideline.
Traditional teaching suggests that in children under 8-10 years of age requiring intubation uncuffed tracheal tubes should be used [1,2]. These should pass through the cricoid portion of the upper airway easily and a leak should be evident at a pressure of around 20 cm H2O [3]. Practically, it is often difficult to find an appropriately sized tube which produces adequate seal for ventilation and an acceptable leak minimising undue pressure on the laryngeal mucosa and surrounding structures. The search for this perfect balance can result in a dilemma: whether to accept large air leak or to insert an oversized tracheal tube.
The background for this practice lies with the understanding that there are fundamental anatomical differences between the airway of an adult and infant. Previously the infant’s airway was thought to be funnel shaped with the narrowest portion at cricoid cartilage being round in shape. However Litman et al [4] report that the cricoid cartilage is in fact ellipsoidal and that the uncuffed tube rests on the posterolateral aspects of this area. This can cause excessive pressure on the adjacent mucosa yet a leak can still occur through the anterior aspect of the cricoid area.
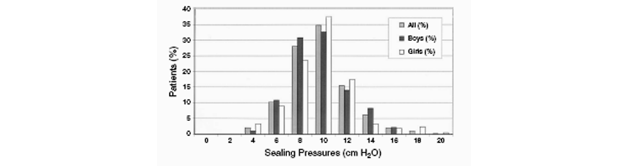
Uncuffed tubes are sealed by the encircling cricoid ring which is called “cricoid sealing”, whereas the cuffed tubes provides tracheal sealing by cuff inflation below the cricoid ring. An appropriate sized circular ETT should fit through this portion without causing a significant leak at modest inspiratory pressures (up to 20cmH20) or too much mucosal pressure resulting in pressure necrosis. In the past concerns have been raised regarding cuffed tubes in that although the ability to ventilate the patient may be enhanced the pressure in the balloon portion may be too high causing pressure necrosis of the surrounding fragile epithelium potentially resulting in permanent upper airway damage such as subglottic stenosis. In a study involving 80 children aged 2-4 years it was found that Microcuff paediatric endotracheal cuffed tubes required significantly lower sealing pressures of 11 cmH2O when compared to other cuffed endotracheal tubes such as the Mallinckrodt, Ruesch, Portex or Sheridan varieties [6]. In a study assessing the Microcuff ETT, 95% of patients achieved a tracheal seal with cuff pressure of less than 15 cmH2O (see figure 1) [12]. In view of these low sealing pressures there was a greater safety margin between this level and higher unsafe limits of more than 25 cm water. A maximum cuff pressure of 20 cmH2O is suggested in this paper [12] though the evidence for this is limited. Further studies may inform our target pressures.
Re-intubation because of excessive air leak has been shown to be a risk factor for the occurrence of airway injury [1] and this is more common when uncuffed ETT’s are utilised.
Sealing pressure of appropriately sized cuffed ETT.(Dullenkopf et al ^12)
Figure 1:
In a recent survey undertaken in the UK only 7% of the lead anaesthetists and 5% of the lead paediatric intensivists in the 30 UK centres with a level 3 PICU routinely used a cuffed tube as a first line ETT in children under 8 years of age 13. The most frequent reason cited for choosing a cuffed tube was reduced lung compliance and inadequate ventilation. It was also found that the cuff pressure was not routinely monitored in these units. The respondents felt that the perceived complications with the use of cuffed tracheal tube were no more common than when using an uncuffed tube. 45% of lead intensivists in this study reported not routinely measuring cuff pressures [13].
Newth et al [11] undertook a prospective observational study of 860 children aged 1 month to 12 years requiring long term intubation admitted to their general and cardiac ICU. The children were intubated with cuffed or uncuffed tube depending on the preference of the physician who intubated. This group used primarily the Malinckrodt ETT’s. They used modified Cole formula ([Age in years/4] + 4) for choosing uncuffed tubes and one half size down for the cuffed tube. Cuff pressures were monitored every 8 hours and maintained at pressures just enough to obliterate the leak at peak inspiratory pressure or up to a maximum of 25 cmH2O. They found no difference in the use of racemic epinephrine, rate of successful extubation or need for tracheostomy between those who were intubated with cuffed and uncuffed endotracheal tube in any age group.
Early paediatric cuffed tube designs had problems with a small margin for error when positioning them which made it relatively easy to have the cuff too proximal to the glottis, hence increasing the risk of glottic damage or the tip of the tube too low resulting in endobronchial intubation. Weiss et al studied the placement of Microcuff paediatric endotracheal tubes with the intubation depth marker as a guide [10]. This allowed adequate placing of the tube with cuff free of the subglottic zone and without risk for endobronchial intubation in children from birth to adolescence. However the evidence for relying on the depth marker has been questioned [16].
Locally we have the portex and microcuff cuffed endotracheal tubes available for use. This guideline is pertinent to the use of all cuffed endotracheal tubes.
A recent study assessed the ETT cuff pressures in 300 patients aged 4 to 92 years who required interhospital transport and found that they had a median cuff pressure of 40 cmH2O (range 10-80 cmH2O) with 64.7% of patients having a pressure of greater than 30 cmH2O [14]. This should be used as a warning to the retrieval team who may be transporting patients with a cuffed ETT sited by the referring centre as mucosal damage has been shown to occur in as short a space of time as 15 minutes in animal models [5]. Currently there is no cuff pressure manometer in the transport bags and staff should be cogniscent of cuff pressures when siting cuffed ETT’s in a distal centre.
There is good evidence from recent studies that manual palpation of the pilot balloon in patients intubated with a cuffed ETT is unreliable in assessing cuff pressures [5, 7, 8, 9] with preponderance for a large overestimation of the pressures generated with pressures over 100 cmH2O recorded in some studies 9. We have also shown in a bench model using a Laerdel Infant mannequin and microcuffed tubes (3.0/3.5/4.0) that as little as 0.2-0.4mls of air is required to generate 20 cmH2O and correlates poorly with manual palpation of the pilot balloon (unpublished data). Most observers greatly under-estimated the pressures generated in the cuffed ETT.
It is therefore essential to monitor ETT cuff pressures for optimal care as part of ongoing patient safety and quality improvement initiatives.
Ideal properties of cuffed paediatric endotracheal tube
- ETT size calculated easily.
- Good outer to inner diameter ratio.
- Low pressure cuff design.
- Cuff distally placed.
Advantages of cuffed endotracheal tube
- Reduced gas leak
- Reduction in the requirement to change the tube
- Improved efficiency of ventilation with minimal air leak
- Reduced risk of aspiration
- Improved accuracy of end-tidal carbon dioxide monitoring
- Greater reliability of spirometry monitoring including tidal volume and lung compliance
- Reduced incidence of autocycling or autotrigerring of ventilator in the flow trigger mode.
- Decreased atmospheric pollution if inhalational anaesthetic in use
- Decreased use of oversized uncuffed tubes in order to avoid leak, which is the main cause of subglottic mucosal ischaemia and ulcerations
- Reduction in potential risk to staff of inhalation of infectious organisms (eg H1N1) whereby
minimal protection (normal surgical mask, not FFP3) are required.
Disadvantages of cuffed endotracheal tube
- Risk of inadvertent cuff overinflation, which can leak to mucosal ischemia and post-extubation morbidity
- A smaller internal diameter ETT is used, compared with uncuffed tubes, which can increase work of breathing in a spontaneously breathing child
- Currently more expensive
Portex cuffed ETT sizing guide:
| Internal diameter | Age in years |
| 5.0 | 2-3 yrs |
| 5.5 | 4-5 yrs |
| 6.0 | 6-7 yrs |
| 6.5 | 8-9 yrs |
| 7.0 | 10-11 yrs |
Recommended sizing guide for Microcuff ETT (Kimberly Clark):
| Internal diameter | Age in years |
| 3.0 | Term to <8 months |
| 3.5 | 8 months to <2 years |
| 4.0 | 2 years to <4 years |
| 4.5 | 4 years to <6 years |
| 5.0 | 6 years to <8 years |
When using a cuffed endotracheal tube it is mandatory that cuff pressure is monitored if inflated. The cuff pressure is traditionally monitored every 6 hours or at least every 12 hours. It is possible to continuously monitor ETT cuff pressures [16]. Some units in addition to monitoring the cuff pressure use a safety device such as “cufflator” or cuff pressure “pop-off” valve so that the cuff pressure never exceeds the set limit. We do not currently use these devices.
Rarely a cuffed ETT may not be inflated for example when a patient is oscillated to maximize CO2 removal; the cuff pressure need not to be monitored in the cuff is deflated.
Equipment needed:
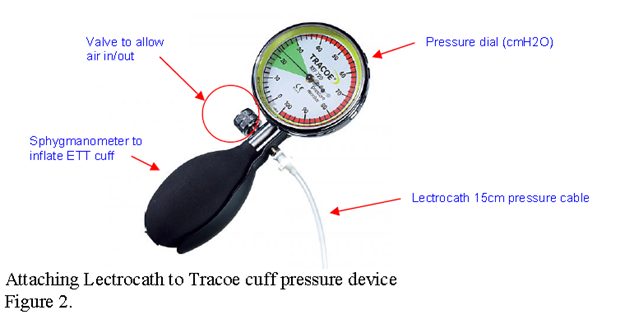
- Lectrocath pressure cabling 15cm (See figure 2) (Ref 1155.01)
- Tracoe Cuff pressure monitor (see figure 2)
- Stored at each bedspace in bedside trolley, each with a unique identifier
- Spare Tracoe cuff pressure monitors are available on shelving in Controlled Drug Room
- Andrew Morley will keep a log of all Tracoe cuff pressure monitors and calibrate them on a monthly basis. Please label any faulty equipment for Bioengineering.
Procedure for cuffed ETT intubation and continuous cuff pressure monitoring:
- Intubation should be undertaken with the cuff in fully deflated position. Cuff should be checked for a leak prior to intubation. If using the Microcuff ETT ensure the green connector attached to the ETT is changed for the hollowed out one that comes in the pack to enable ETCO2 attachment. (This is being changed at the factory so that this will become standard set-up following our feedback.)
- It should be possible to produce a leak at a maximum inspiratory pressure of 20 cm water with the cuff fully deflated. If there is no leak at a peak inspiratory pressure of 20 cm water, then it is important to downsize the ETT.
- The cuff is inflated gradually, using the bedside “tracoe” cuff pressure device with a closed valve (see figure 2) until there is no leak at the lowest cuff sealing pressure (maximum ETT cuff pressure of 20 cmH20 should be used). If a cuff pressure of greater than 20 cmH20 is required then this indicates that the ETT and its cuff are too small, requiring excessive cuff inflation and the ETT should be upsized.
- Fill in CIS intubation procedure form documenting whether tube is cuffed or uncuffed and whether cuff inflated or not and at what pressure cuff is inflated.
- This should be undertaken for all cuffed ETT’s where the cuff is inflated.
- The cuff pressure should be checked every 6 hours at least. Oropharyngeal suction should be undertaken prior to the deflation of the ETT cuff to minimse risk of aspiration. If the cuff pressure is greater than 20 then release air from cuff via valve on left of “tracoe” device (see figure 2).
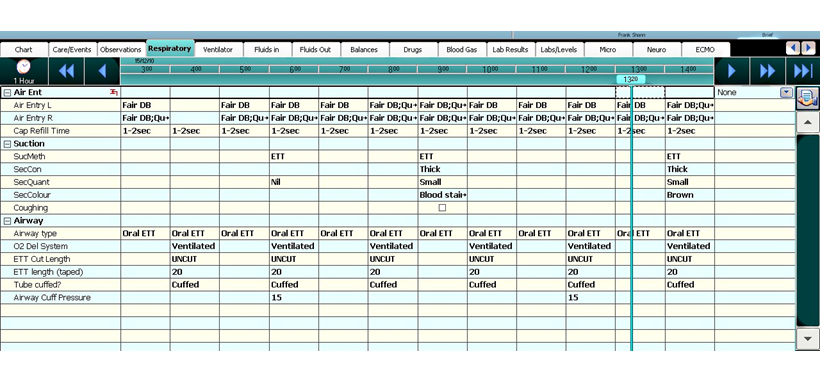
- Cuff pressures should be routinely documented on the respiratory chart in CIS (figure 4).
- Cleaning of Tracoe cuff pressure monitor should be undertaken as directed by the “GG&C Decontamination Policy and the Standard Operating Procedure for the Cleaning of Near Patient Healthcare Equipment” for most circumstances detergent wipes are satisfactory. For equipment used with a patient in source isolation, including cohort patients 1,000ppm, “Actichlor plus” should be used.
- A cuffed ETT with a burst cuff may need to be changed for a new cuffed ETT. Please fill in a Datix form if this occurs.
- Cuffed ETT’s should always be placed with cuff fully deflated (unless deflated when patient oscillated to maximize CO2 removal)
- On intubation inflate cuff to max pressure of 20cmH2O to minimize leak around ETT
- Record cuff P on intubation record and on CIS “respiratory” page (see fig 4)
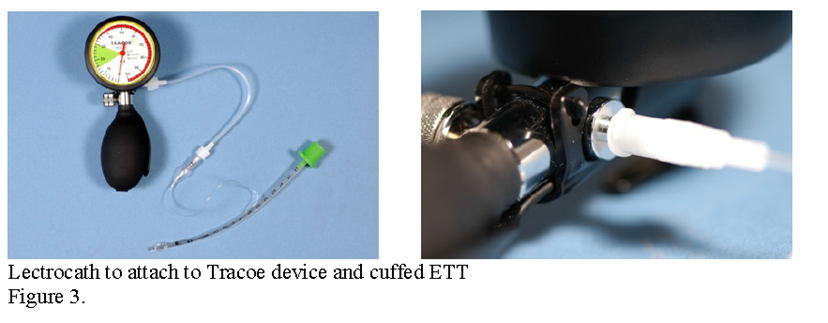
- Check cuff P by attaching Tracoe cuff pressure device as shown in figure 3 to ETT cuff pilot balloon
- Connect Lectrocath to Tracoe cuff P device and ETT cuff valve (fig 3)
- Close valve
- Inflate cuff to max pressure of 20cmH2O
- If Cuff P >20cmH2O then release air from cuff using valve (fig 2)
- Disconnect Lectrocacth from cuffed ETT between cuff P checks.
- Check Cuff pressure every 6 hours and document on CIS “Respiratory” page
- Weiss M, Dullenkopf A, Fischer JE, Keller C, Gerber AC. Prospective randomized controlled multicentre trial of cuffed or uncuffed endotracheal tubes in small children. Brit J Anaesth 2009;103(6):867-73
- Weber T, Salvi N, Orliaguet G, Wolf A. Cuffed vs non-cuffed endotracheal tubes for paediatric anaesthesia. Ped Anaesthesia 2009;19(S1):46-54
- American Heart Association. Part 12 Pediatric advanced life support. Circulation 2005;112:167-87
- Litman RS. Weissend EE. Shibata D. Westesson PL. Developmental changes of laryngeal dimensions in unparalyzed, sedated children. Anesthesiology. 2003;98(1):41-5
- Fernandez R, Blanch L, Mancebo J, Bonsoms N, Artigas A. Endotracheal tube cuff pressure assessment: pitfalls of finger palpation and need for objective assessment Crit Care Med 1990;18:1423-6
- Dullenkopf A, Schmitz A, Gerber AC, Weiss M. Tracheal sealing characteristics of pediatric cuffed tracheal tubes Ped Anesth 2004;14:825-30
- Janossy KM, Pullen J,Young D, Bell G. The effect of pilot balloon design on estimation of safe tracheal tube cuff pressure. Anesthesia 2010;65:785-791
- Morris LG, Zoumalan RA, Roccaforte JD, Amin MR. Monitoring tracheal tube cuff pressures in the intensive care unit: a comparison of digital palpation and manometry. Annals of Otology, Rhinology & Laryngology. 2007; 116(9):639-42.
- Parwani V, Hoffman RJ, Russell A, Bharel C, Preblick C, Hahn IH. Practicing paramedics cannot generate or estimate safe endotracheal tube cuff pressure using standard techniques Prehospital Emergency Care. 2007;11(3):307-11.
- Weiss M. Balmer C. Dullenkopf A. Knirsch W. Gerber ACh. Bauersfeld U. Berger F. Intubation depth markings allow an improved positioning of endotracheal tubes in children. Canadian Journal of Anaesthesia. 2005;52(7):721-6.
- Newth CJL, Rachman B, Patel N, Hammer J. The use of the cuffed versus uncuffed endotracheal tubes in paediatric intensive care. J Pediatr 2004;144:333-7
- Dullenkopf A, Gerber AC, Weiss M. Fit and seal characteristics of a new paediatric tracheal tube with high volume-low pressure polyurethane cuff. Acta Anasthesiol Scan 2005;49:232-7
- Flynn PE, Black AE, Mitchell V. The use of cuffed tracheal tubes for paediatric tracheal intubation, a survey of specialist practice in the United Kingdom. Eur J Anaesthes 2008;25:685-8
- Chapman J, Pallin D, Ferrera L, Mortell S, Pliakas J, Shear M, Thomas S. Endotracheal tube cuff pressures in patients intubated before transport. Am J Emerg Med 2009;27:980-2
- Nordin U. The trachea and cuff induced tracheal injury: an experimental study on causative factors and prevention. Acta Otolaryngol 1976;345 (Sup 345):1-7.
- Whyte K, Levin R, Powls A. The optimal positioning of endotracheal tubes in neonates. The Scottish Medical Journal 2007; 52(2): 25-27.
Last reviewed: 24 November 2020
Next review: 30 November 2023
Author(s): Dr V Mani, Mr A Morley, SN R Reardon, Dr M Davidson, Dr N Spenceley, D R Levin

