ICP monitoring SOP
exp date isn't null, but text field is
Objectives
The objective of this document is to provide a detailed Standard Operating Procedure for the insertion of ICP monitoring.
Scope
This standard operating procedure (SOP) is intended for all healthcare professionals caring for patients with an ICP monitor in the Paediatric Intensive Care Unit at the Royal Hospital for Sick Children, Glasgow
Audience
All medical, nursing and allied professionals caring for patients who have an ICP monitor should be familiar with the SOP.
a) Definition
Intracranial Pressure (ICP) monitoring is a tool used to help assess the balance of the intracranial contents (brain, blood and CSF). This is achieved by inserting a pressure-sensitive probe into the brain matter. The monitor converts the pressure to a waveform display and corresponding numeric value, to represent the pressure inside the skull.
b) Indications
ICP is monitored to allow active management of the intracranial contents when there is –
- Head injury
- Intracranial haemorrhage
- Coma
- Likelihood of post-operative swelling
c) Causes of Raised ICP:
Increased blood volume
- Increased cerebral blood flow (hypoxia and hypercarbia both cause a decrease of blood vessel tone allowing a greater blood flow to compensate for reduced oxygen levels in the blood, or greater blood flow to remove increased carbon dioxide levels).
- Increased venous volume (from venous outflow obstruction).
- Increased intrathoracic pressure (generating venous congestion) – e.g. coughing.
- Head-down position.
Increased brain substance
- Tumour
- Intracerebral bleeding
- Infection
- Swelling
Increased CSF
- Communicating hydrocephalus
- Obstructive
d) Symptoms and Signs of Raised Intracranial Pressure (ICP)
Infants
- Irritability
- Vomiting
- Full, bulging fontanelle
- Neurological symptoms – decrease in GCS, cranial nerve palsy, sun-setting eyes (eyes unable to look up)
- Irregular respirations & apnoeic periods
- Splaying of cranial sutures, a big head – measure head circumference regularly
- Tachycardia /Hypertension /Bradycardia
- Pupil changes (fixed pupils, irregularly shaped pupils or dilated pupils all worrying)
Older children
- Headache
- Nausea, vomiting
- Lethargy
- Irritability
- Worsening concentration
- Decreased GCS
- 6th nerve palsy
- Other abnormalities – seen at neurologic exam
- Tachycardia /Hypertension/ Bradycardia
- Pupil changes (fixed pupils, irregularly shaped pupils or dilated pupils all worrying)
e) Complications of ICP Monitoring
- Infection
- Haemorrhage
- Haematoma
Prior to insertion FBC, clotting and Group and Save should be performed.
f) Cerebral Perfusion Pressure (CPP)
Measurement of ICP allows calculation of CPP which is an indication of blood flow.
CPP =MAP* – ICP
*MAP (Mean arterial pressure)
Sometimes a CPP will be set as a goal. For each individual patient a target ICP and CPP should be agreed by intensivist and neurosurgeon. For normal values see Interpretation of ICP Monitoring.
The ICP monitoring bolt is inserted by a Neurosurgeon as a sterile procedure. This procedure may be performed in the PICU and will require anaesthesia. All equipment will be found in the Neuro ICP trolley.
The surgeon will require
- Dressing trolley, cleansed
- Gown and hand towel
- Surgeons gloves
- Sterile drapes
- Hernia towel
- Dressing pack
- Betadine Solution / Chlorprep (surgical preference)
- 5ml syringe
- Normasol
- Green spinal needle
- Blue needle
- Lidocaine 2% 5ml.
- Scalpel
- Raumedic ICP catheter pack
- Hand held drill (from Theatres – Out of hours – Page 8502 for code for theatre. Drill located in Theatre 7.)
- NPS-2 zero point module and Raumedic extension cable
- Phillips Pressure module (labelled ICP – Neuro trolley)
- Hand-held suture
Procedure
- The area chosen for insertion will be shaved, then cleansed with Betadine /chloraprep Solution.
- Local anaesthetic is infiltrated.
- Sedation and/or analgesia may be given prior to the next steps.
- A small burr hole will be drilled through the skull. The nurse must hold the patient’s head steady whilst the Neurosurgeon performs this task.
- The securing "bolt" is screwed into the skull.
- The catheter will require to be zero-referenced before insertion : See photographic set-up guide on next page
- The Neurosurgeon will moisten the tip of the catheter by gently wiping the tip with gauze soaked in Normasol.
- The catheter can now be inserted through the burrhole.
- The catheter is secured to the scalp with a suture.
- The bolt is wrapped in Betadine-soaked gauze or Chloraprep to minimise any infection risk.
- The orange cap and bolt kit (supplied) should be kept at the bedside – these are required when monitoring is discontinued and to remove the bolt . Place in plastic bag labelled ICP and tape to bed/cot.
- Presence of this kit should be checked once per shift.
- If the ICP monitor was placed in theatre the bolt kit should return with patient. Check that this is present. See below.

Prior to EVERY use, the zero point module (NPS2), Raumedic extension catheter and Raumedic ICP catheter must be visually inspected for damage (see fig 1, 2&3*). If damage has been found, in any of the products the equipment should be returned to Clinical Physics and new equipment used.
The Raumedic catheter MUST be zero-referenced before insertion and following every disconnection, As shown below:
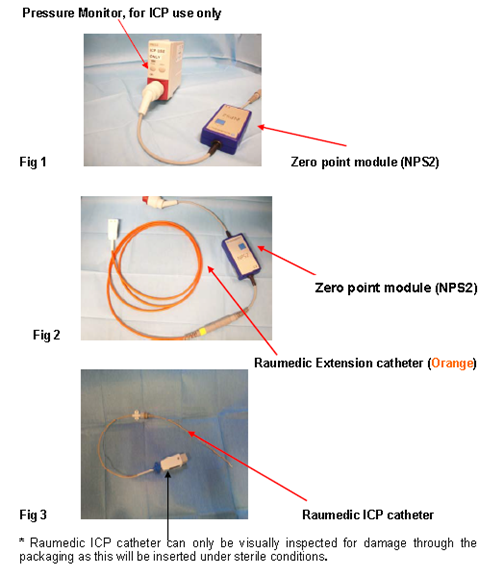
Connect the Raumedic extension catheter cable (orange) to the Raumedic ICP catheter, lining up the gold dots on both halves of the white connector (See Fig 4 & 5).
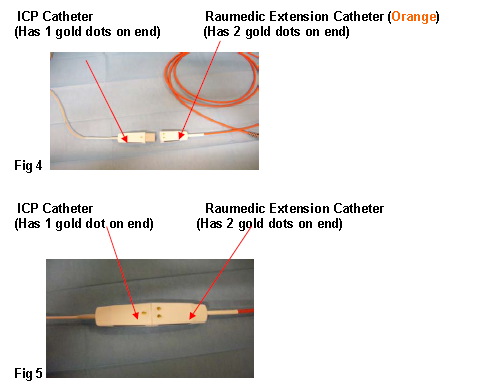
WARNING: if forced, it is possible to reverse the connector (gold dots not lined up on the two halves)-this will cause a large over-reading of the ICP (up to 50mmHg).
Connect the Raumedic Calibration box Interface Cable to the bedside monitor, using the PHILLIPS pressure Modules marked for ICP use only (See Fig 6).
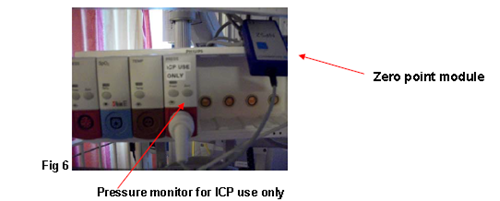
NB: Pressure modules labelled for ICP use only should used for ICP monitoring. Studies have shown that other pressure modules used to monitor ICP have caused a large over-read.
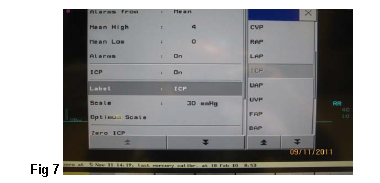
Select ICP label on Phillips monitoring (See Fig 7)
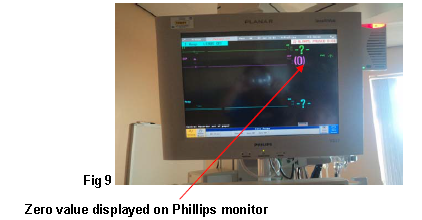
Press and hold blue zero button on the Zero point module (NPS2) and at the same time set the Phillips monitor to read zero in standard way, only release blue zero button when monitor reads zero (See Fig 8 & 9).

Only release blue button when zero value displayed (See Fig 9).
If ICP bolt being inserted on PICU
Patient will require anaesthesia.
Neurosurgeon may require assistance with positioning of the head.
All equipment required is found in Neuro ICP trolley. Drill will need to obtained from theatre.
At point of insertion ask doctor to hold tip of catheter in approximation to the physiological zero reference point if possible (external auditory meatus). Keep the tip away from direct light. Wait at least 10 seconds and confirm that the catheter reads 0mmHg (=/- 2mmHg). If deviation is greater, use another catheter and send the first one to Biomedical Engineering as per management of faulty equipment.
NB: Remember this is a sterile procedure.
Re-zeroing of the ICP monitoring will be required post theatre and following disconnection of the monitor (see Fig 4 to 9 above).
- Monitor and record GCS 2 hourly.
- Monitor and record ICP and CPP .
- Ensure bolt is dressed with Betadine-soaked/ chlorhexidine swabs, and change daily (record CIS).
- Observe site for signs of leakage, haematoma formation or infection, and report abnormalities to medical staff.
- Nurse patient in 30 degree head-up position.
- Position head and neck in anatomical neutral position.
- Avoid lying patient on side that bolt is located.
- Carefully position ICP catheter, avoiding tension or traction. Avoid, where possible, activities that increase ICP. Consider sedation boluses ( Fentanyl 2micrograms/kg IV) pre-intervention or endotracheal instillation of lignocaine 1% (max 2mls) pre-physio.
- Record any activities that significantly affect ICP as events eg. Suction, movement.
- Administer prescribed medication to achieve and maintain targets for ICP, MAP and CPP.
- See Traumatic Brain Injury Guideline for management of raised ICP
|
Age
|
Normal ICP values
|
Treatment Threshold for ICP |
Target CPP values
|
|
Neonates (or infants with wide fontanelle)
|
1.5 – 5 mmHg
|
>10 mmHg
|
>30mmHg
|
|
0-2 years
|
3 –7 mmHg
|
Remains unknown but >20mmHg (possibly 15mmHg)
|
>40mmHg
|
|
2-10 years
|
3 – 7 mmHg
|
>20mmHg
|
>50mmHg
|
|
>10 years
|
<10 – 15 mmHg
|
>20mmHg
|
>60mmHg
|
Agree threshold for ICP and CPP intervention for each individual patient with intensivist and neurosurgeon.
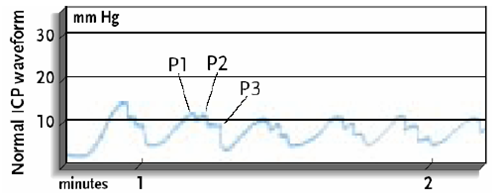
ICP monitoring waveform has a flow of 3 upstrokes in one wave.
P1 = (Percussion wave) represents arterial pulsation
P2 = (Tidal wave) represents intracranial compliance
P3 = (Dicrotic wave) represents aortic valve closure
In normal ICP waveform P1 should have highest upstroke, P2 in between and P3 should show lowest upstroke.
On eyeballing the monitor, if P2 is higher than P1 - it indicates intracranial hypertension.
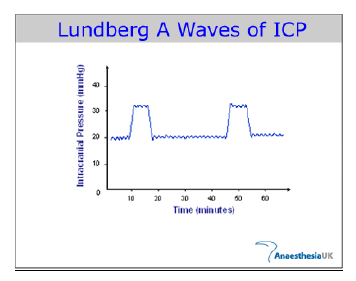
Lundberg A waves "or plateau waves" are steep increases in ICP lasting for 5 to 10 minutes. They are always pathological and represent indication of early brain herniation.
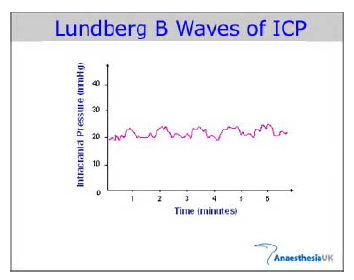
Lundberg B waves are oscillations of ICP at a frequency of 0.5 to 2 waves/min and are associated with an unstable ICP. Lundberg B waves are possibly the result of cerebral vasospasm, because during the occurrence of these waves, increased velocity in the middle cerebral artery can be demonstrated on transcranial Doppler.
This is carried out by the Neurosurgeon using the retained bolt kit (should be in plastic bag taped to bed/cot)– the catheter is unscrewed following the instructions.
The surgeon will require
- Dressing trolley, cleansed
- Dressing pack
- Sterile gloves
- Betadine Solution or Chloraprep
- Bolt kit (retained from insertion)
- Hand-held suture
- Mepore dressing
Above all present in Neuro ICP trolley.
The patient may or may not require the insertion site to be sutured.
Some patients will have an ICP monitor inserted to help plan for further surgery or to evaluate the effectiveness of previous surgery. These patients will generally be relatively well patients in whom there are some concerns that chronic raised intracranial pressure may be an issue.
The ICP bolt is placed as before but this time the patient is connected to a Speigelberg monitor. This acts rather like a cardiac Holter monitor. It records the ICP over a period of days whilst the patient undertakes various activities. Events must be recorded.
In these cases there is generally no intention to intervene to changes in ICP whilst recording. This is purely an information gathering process. Obviously if the patient becomes unwell the ICP may be relevant and appropriate action taken.

Last reviewed: 20 April 2014
Next review: 20 April 2016
Author(s): J. Richardson, H. Gavin, INS
Reviewer Name(s): Anne McGettrick & Roddy O’Kane

