Underwater seal chest drainage in the highly dependent or critically ill infant or child: nurse role: ongoing chest drain management
Objectives
Chest drains and chest drainage systems are used frequently in the paediatric critical care unit. There are many reasons for chest drain insertion but primarily they are used whenever there are specific conditions that interfere with the normal mechanism of lung expansion and altered intrathoracic pressures.
Pleural chest tubes are inserted to evacuate blood, pus, air and fluid, from the thoracic cavity, to re-establish negative pressure in the intra pleural space and thereby expand the lungs following collapse resulting from surgery or trauma.
Mediastinal chest tubes are placed in the mediastinum following open heart surgery, via a medial sternotomy in order to prevent accumulation of blood and clots around the heart, which could cause cardiac tamponade – a life threatening situation.
There are many different types of chest drains available including one-way flutter valve drains such as the Heimlich device or portable drains. However, for the majority of patients in the paediatric critical care unit an underwater seal chest drainage system will be used. These systems provide an underwater seal, fluid collection chamber and suction chamber.
In paediatric intensive care it is normally the physician or Advanced Nurse Practitioner who inserts chest drains. However, the bed side nurses’ role is pivotal in ensuring the patient is cared for safely throughout the insertion procedure.
This guideline is intended as a resource for staff involved in caring for children in Paediatric Critical Care 1D (PICU) that require chest drain insertion. The guideline has been constructed after literature search and review of sourced textbooks, national guidelines & recommendations British Thoracic Society, Medline and CINHAL, and external nurse expert peer review and opinion.
Further information on chest drainage in: ‘Tutorial Notes-Chest Drainage’ Maxwell (2018) and additional chest drain system resource at: www.atriummed.com/ See also recommendations and precautions.
Scope
This nursing procedural guideline is intended to be followed by nurses involved in caring for the highly dependent or critically ill infant or child requiring underwater seal chest drainage within the Paediatric Critical Care Unit 1D (PICU) at the Royal Hospital for Children, Glasgow.
Audience
All nursing staff involved in caring for infants or children requiring underwater seal chest drainage in Paediatric Critical Care (PICU) should be familiar with this nursing procedural guideline.
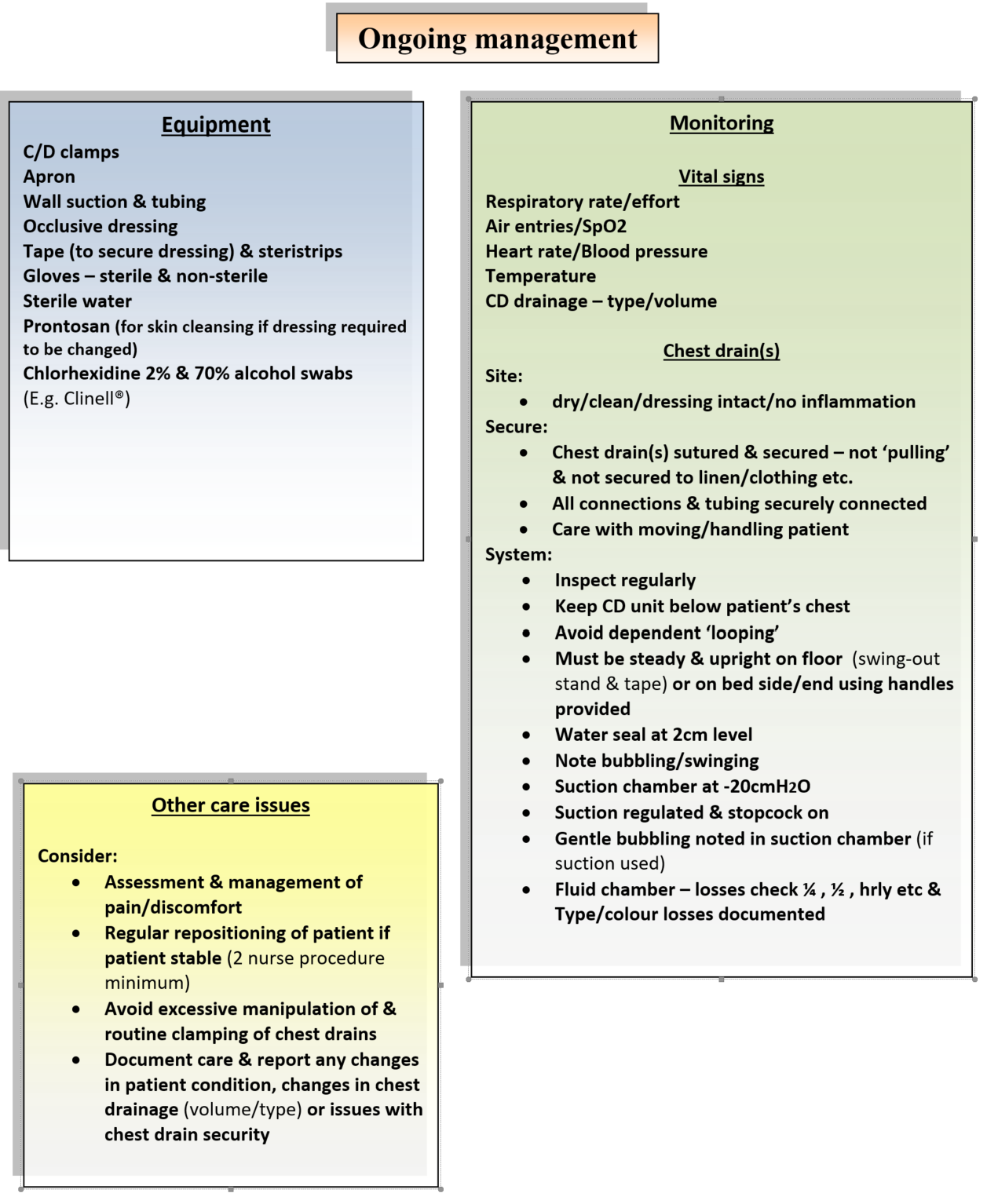
Equipment: Available for ongoing management or in case of any untoward event
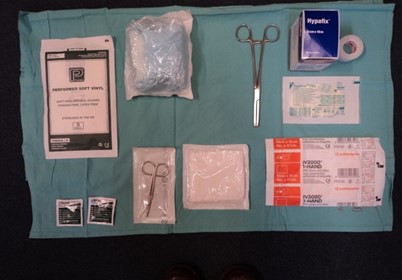
Fig. 1. Bed side equipment for ongoing chest drain management
Available at bed side:
- Clamps (x1 each drain)
- Suction tubing-if required
- Suitable dressing (for ongoing site care)
- Sterile gloves
- Sterile water
- Sterile scissors
- Disposable apron
- Disposable gloves
- Wall suction gauge-if required (low flow * Fig. 2)
SAFETY PACK:
- Chest drain site occlusive dressing (E.g. Duoderm®)
- Steri-strips
- Chlorhexidine 2% & 70% alcohol (swab suitable for urgent event-Clinell)
On chest drain trolley:
- Chest drain system

Fig. 2. *Low flow suction unit
|
PROCEDURE: Ongoing chest drain management |
RATIONALE |
|
Vital signs & patient observations: The infant or child with a chest drain(s) in situ must have the following observations monitored frequently & documented:
If a suitable invasive monitoring line is in situ then regular arterial or venous blood gases should be done. |
Frequent monitoring of vital signs is important in detecting any alterations from previously documented normal values as these may indicate problems such as haemorrhage, unresolved pneumothorax, tension pneumothorax, sepsis, infection and ventilation-perfusion mismatch. Suggestions for monitoring vital signs ranges from ¼ hourly immediately post drain insertion/admission, to ½ hourly to hourly whilst drain is in situ. The frequency of monitoring specific vital signs and blood gas analysis will be determined by the child’s clinical status with any deterioration in the child’s vital signs being reported to the nurse-in-charge and medical team immediately. |
|
Chest drain site care: the nurse must ensure the drain site is checked regularly for the following:
|
The drain must be well secured after insertion to prevent it becoming dislodged, slipping or falling out. Large amounts of tape and padding may restrict chest movement and prevent regular inspection of the drain site for complications. A dry non-adherent dressing, non-occlusive is most suitable. The drain site and dressing should be reviewed daily and the dressing should not need redressed for 2-3 days unless leakage apparent. Any signs of complications such as infection should be documented and reported and appropriate action taken. E.g. wound swab or medical team review. |
|
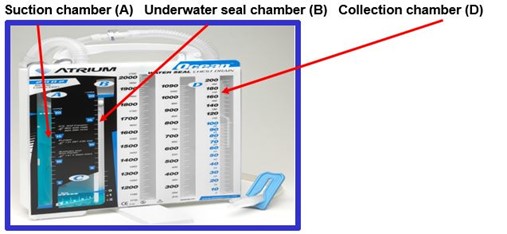
Chest drainage unit (CDU) care: the nurse must check the under water seal chest drainage system frequently to ensure it is working correctly and to avoid potential problems: *see (Fig. 3) Keep chest drainage system and tubing below the level of the patients chest
Perform initial inspection of connections & tubing. Thereafter inspect CDU tubing & drain connections regularly (suggested hourly) and keep tubing free from bedsides/cot-sides Ensure tubing & drain(s) are secure but not ‘pulling’. Try not to secure tubing to child’s bed, linen or loose clothing (Fig. 4) Aim to lay tubing horizontally across bed before dropping it vertically into drainage system to facilitate drainage – avoid dependent ‘loops’ or kinking of tubing (Fig. 5) Ensure chest drainage unit is secured upright on floor beside or at the end of the bed/cot. |
The chest drainage system must always be kept below the level of the child’s chest to prevent fluid re-entering the pleural space – syphonage.
Regular inspection of the drain and tubing is vital to ensure that the system is still intact the drain has not slipped, connections have not come loose or tubing has become kinked. Securing tubing to clothing or bedding is not advised as sudden movements by the child or change of bed-linen could dislodge the drain. Dependent loops or kinking of tubing can impede drainage, block tubing and cause high pressures at chest tube and drainage tube connections, potentially resulting in clinical complications such as tension pneumothorax. Securing the drainage system to the floor with tape may be necessary to prevent tipping of system. |
|
Check water seal chamber (B) (Fig. 3) maintained at 2cm level Monitor and record any ‘bubbling’ or ‘swinging’ in the water seal chamber of the CDU. Report any changes to nurse-in-charge. If chest drain in pleural cavity, observe and record any fluctuations in water seal level of CDU with respiratory effort/ventilation – ‘tidalling’ Ensure suction chamber (A) (Fig. 3) filled to -20cmH2O level in CDU. If suction required - Check suction tubing connected to low flow regulated suction & suction control stopcock at CDU switched on. Check negative pressure on suction is set low enough to give gentle bubbling in the suction chamber – no excessive bubbling Ensure suction filter attached – changed when indicated Check fluid collection chamber (D) (Fig.3) frequently (*15 min. intervals to 30min., then hourly) and document volume, type and colour of drainage. E.g. fresh blood, serous, cloudy. Always label chest drain(s) and drainage units clearly. E.g. Left (L) pleural 1 or Right (R) mediastinal 2.
|
Water in the water seal chamber (B) (Fig. 3) can evaporate and under water seal will be lost. The level must be checked regularly and ‘topped-up’ as per manufacturers instructions. Persistent bubbling may suggest visceral pleural air leak, a drain on suction that has one of the drain eyelets open to air or with mediastinal drains patient with ‘open’ chest. ‘Swinging’ of the water seal level with respirations indicates drain patency and confirms drain position in pleural cavity.
If suction is required, a low pressure system must be used as excessive negative pressures may cause perpetuation of air leaks. If suction is required for more than one chest drain then a separate suction unit is advised for each chest drain. Turbulent bubbling is unnecessary, will not improve fluid drainage and will result in increased evaporation of water in the chamber.
Frequent assessing and documenting of fluid volume and type drained and from what site is essential, as this may help the nurse determine if the child has any of the following:
*Frequency of checking tubing and drainage will range from every 15 minutes initially (for first 6 hours) post admission from cardiac or thoracic surgery, to 30 minutes (6 hours) then hourly once child stabilised. This is provided there is no other evidence or suspicion of bleeding or tamponade present. |
|
Specific nursing care issues:
|
Pain from having a chest drain in situ can inhibit the child’s movement and breathing which can slow their recovery. Therefore, regular pain assessment is vital to ensure the child receives adequate analgesia while the drain is in situ. Repositioning and improving mobility can facilitate drainage, aid breathing and lung expansion and reduce complications associated with immobility. Repositioning the infant/child with a chest drain in situ should involve at least two nurses in order to prevent accidental disconnection or kinking of drain and/or tubing. Routine manipulation of chest drain tubing by ‘milking’ or ‘stripping’ the tubing has been common practice in the past in an attempt to prevent mediastinal drains from blocking with clots and causing cardiac tamponade. However, this type of tubing manipulation is thought to cause significant increases in negative intrathoracic pressures, may not be of proven benefit and may cause tissue damage. Routine clamping of chest drains is not recommended especially if bubbling, as it prevents the escape of air or fluid from the chest or mediastinum, leading to an increased risk of tension pnuemothorax or cardiac tamponade. |
Fig.3. Underwater seal chest drainage unit
|
Fig.4 Tubing secure
|
Fig.5 Avoid dependent loops (Elevation of cot/bed –as above - should also aid drainage) |
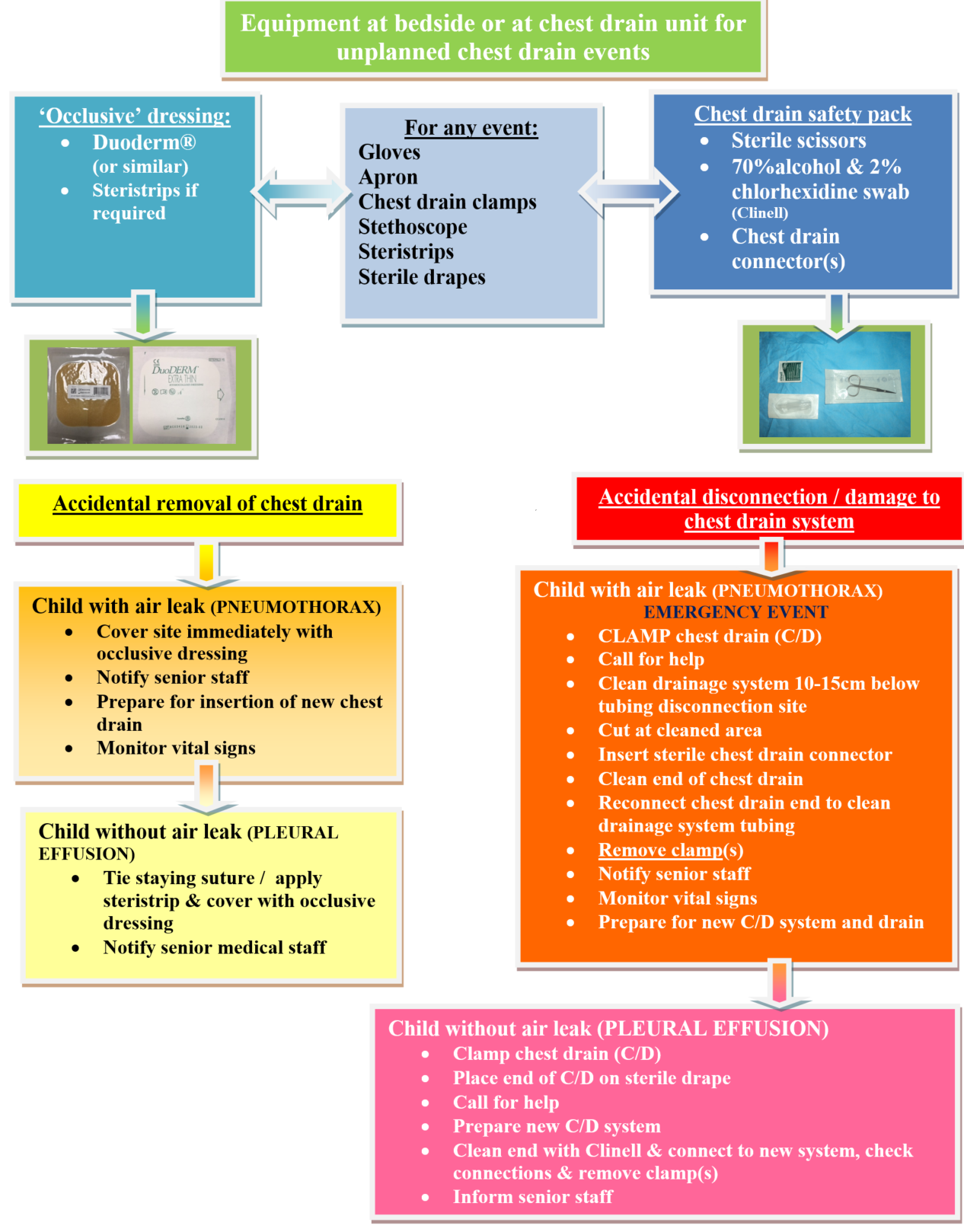
Available for ongoing management or in case of any untoward event. (Equipment available at bed side or on *chest drain trolley)
- Gloves (for all contact with chest drains)
- Apron (for all contact with chest drains)
- 70% alcohol & 2% Chlorhexidine swabs (E.g. Clinell® swabs)
- Chest drain clamps
- Sterile scissors
- Stethoscope
- Spare connector – correct size (attached to back of chest drainage system) Occlusive dressing:
- Occlusive dressing: e.g. Duoderm®
- Steri-strips
- New underwater seal system*
- Sterile water*
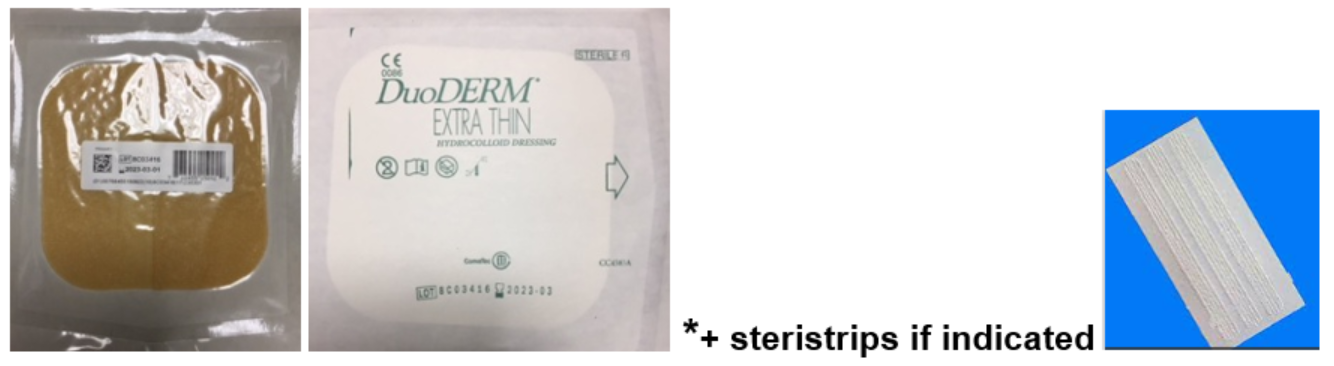
A. Occlusive Seal Dressing (Fig 6)
To be kept in bed side trolley & attached to back of chest drain system of every child with chest drain insitu. Occlusive seal dressing example: Duoderm® & steristrips
Fig 6.
 B. Chest Drain Safety Pack
B. Chest Drain Safety Pack
To be attached to the back of the chest drain collecting chamber of every child with chest drain insitu (Fig. 7 & 8). To include – appropriately sized chest drain connector, scissors, Clinell® swabs (Fig.1, 7 & 8)
|
Fig. 7 |
Fig 8. |
CHILD WITH AIR LEAK (E.g. Pneumothorax)
|
PROCEDURE |
RATIONALE |
|
Quickly cover chest drain site/wound with an occlusive seal dressing - Duoderm®* (*Occlusive dressing for accidental removal of chest drain) (Fig.6) |
This will provide an occlusive seal and help prevent air being introduced into pleural space during respiration.
|
|
Notify medical & senior nursing staff immediately |
To formulate a plan for ongoing management |
|
Prepare for reinsertion of chest drain |
Equipment required at bedside, to aid prompt chest drain re-insertion |
|
Careful observation of child’s respiratory and cardiovascular status |
To monitor for symptoms of increasing pneumothorax and / or tension pneumothorax |
Fig. 6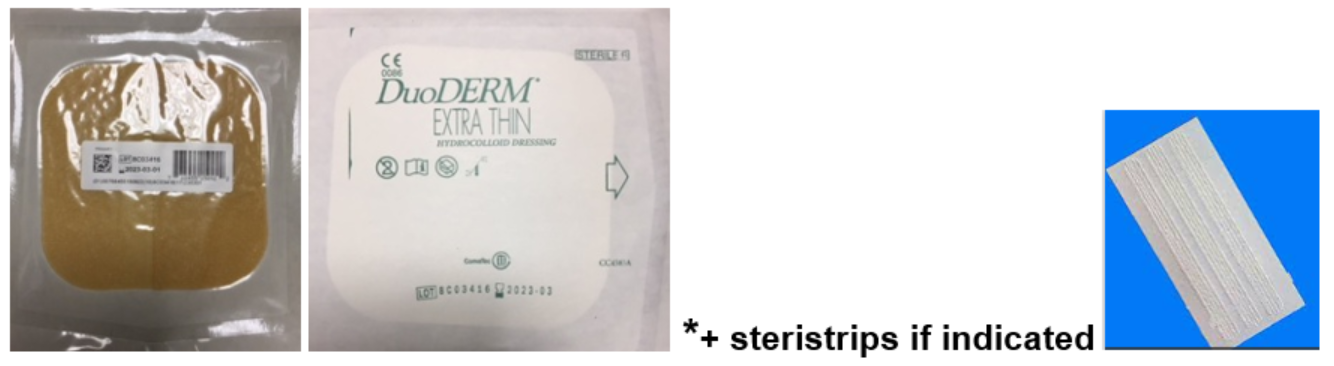
CHILD WITHOUT AIR LEAK (E.g. Pleural effusion)
|
PROCEDURE |
RATIONALE |
|
Tie staying suture if present and cover site with A. Occlusive seal dressing-Duoderm®* (*Occlusive dressings for accidental removal of chest drain) (Fig.6) If no staying suture present, then use steri-strips to close chest drain wound site. Then cover site with Duoderm® (Fig. 6) |
This will provide an occlusive seal and help prevent air being introduced into pleural space during respiration.
|
|
Notify medical and senior nursing staff immediately |
To formulate a plan for ongoing management |
|
Careful monitoring of child’s respiratory status |
To monitor for symptoms of increasing pleural effusion. |
|
PROCEDURE |
RATIONALE |
|
Clamp chest drain |
To prevent air being introduced into pleural space during respiration EMERGENCY SITUATION It is generally contraindicated to clamp a chest drain with an air leak, however in this emergency the chest drain MUST be clamped, to prevent air being drawn into the chest, but for the shortest time possible |
|
Call for help |
|
|
Using equipment from B. Chest drain safety pack (Fig. 7 & Fig. 8) Clean chest drainage system tubing approximately 10-15cm below tubing disconnection site with Clinell® swab. Using sterile scissors cut the tubing at the cleaned area. Insert sterile (appropriately sized) chest drain connector to the cut and clean tubing. Clean end of chest drain with Clinell® swab. Reconnect chest drain to cleaned tubing and connector and remove clamp |
To reduce potential of infection To remove portion of tubing contaminated during disconnection To reduce potential of infection and ensure good seal To reduce potential of infection To re-establish underwater drainage system |
|
Prepare new drainage system Ensure connections are secure Secure drainage container to the floor |
To prevent infection
|
|
Inform medical and senior nursing staff |
To formulate a plan for ongoing management |
|
PROCEDURE |
RATIONALE |
|
Clamp chest drain |
To prevent air being introduced into pleural space during respiration |
|
Place drain end on sterile drape |
To prevent infection |
|
Call for help |
|
|
Prepare new drainage system |
To prevent infection |
|
Clean drain end with Clinell® swab Connect to drainage system, remove clamps Ensure connections are secure Secure drainage container to the floor |
To prevent infection To re-establish underwater drainage system |
|
Inform medical and senior nursing staff |
To formulate a plan for ongoing management |
|
PROCEDURE |
RATIONALE |
|
Regular assessment of chest drain site |
To recognise signs of skin deterioration or infection (exudate, odour, redness, swelling) |
|
If infection suspected -
|
To ascertain if infection is present |
|
Apply dressing to chest drain site according to hospital wound chart or contact Tissue Viability Nurse for wound assessment |
To provide evidence based wound care and promote healing |
|
Document wound management plan, by completing wound chart |
To provide continuity of wound care |
|
Re-assessment of wound as documented in wound chart |
To evaluate effectiveness of treatment |
|
Utilise sterile technique when dressing / manipulating chest drain |
To prevent infection |
|
PROCEDURE |
RATIONALE |
|
Monitor chest drain losses for signs of infection |
To recognise infection |
|
Obtain sample of chest drain loss Sampling of patient drainage must be in accordance with approved hospital infection control standards. Wash hands, don apron and gloves before either procedure. Sample Collection Procedure - (needle-free) Sample to be taken from drainage system tubing, not collecting chamber
Sample Collection Procedure – (with needle) In chest drain systems without a sampling port (E.g. Atrium 2002), sample must be aspirated from drainage system tubing using a needle.
Then follow steps v. & vi. above. |
To ascertain if infection is present
Selected models of chest drain systems (E.g. Atrium 2012) include a needleless luer port on the patient tube connector for sampling patient drainage. (Fig. 9 & Fig 10)
Fig. 9
Fig. 10 ALL CHEST DRAIN SYSTEMS SHOULD BE NEEDLE-FREE. However, if you have a system that is not, use the following procedure: *Do not puncture chest drain system tubing with an 18g or larger needle.
Fig. 11 |
|
Monitor child for signs of systemic sepsis
|
To ascertain if localised infection has become systemic infection. To formulate a management plan |
|
PROCEDURE |
RATIONALE |
|
Monitor chest drain losses at regular intervals. E.g.
Or as required by child’s clinical condition |
To ascertain sudden cessation in drainage
|
|
Position chest drain tubing to prevent dependant loops and coiling by laying tubing along bed dropping vertically into drainage chamber (Fig. 12) |
To prevent clot formation and blockage of tubing |
|
Monitor chest drain and tubing for clot formation and blockage Position tubing over bed covers to allow constant observation
|
Blockage of chest drains can lead life-threatening complications
leading to haemodynamic and respiratory compromise |
|
Inform medical & senior nursing staff of clot formation or blockage of chest drain and tubing
|
To formulate a plan for ongoing management Stripping of chest drains with mechanical rollers is a technique used to clear the tubing of clots and blockages, by generating short bursts of negative pressure to the drain. This is a controversial technique and should only be undertaken under senior nurse & medical staff supervision. |

Fig. 12
Practical chest drainage system issues: When there is no air leak, the water level in the water seal chamber should rise and fall with the patient's respirations, reflecting normal pressure changes in the pleural cavity during respiration. During spontaneous respirations, the water level should rise during inhalation and fall during exhalation. If the patient is receiving positive pressure ventilation, the oscillation will be just the opposite. Oscillations may be absent if the lung is fully expanded and suction has drawn the lung up against the holes in the chest tubes.
A patient with mediastinal chest tubes (and a ‘closed’ chest) should have no bubbling or fluctuations in the water seal chamber. As one of the risks of accumulation of fluid, blood or clots around the heart is cardiac tamponade, it is particularly important for nurses caring for patients with mediastinal chest tubes to be watchful for signs of cardiac tamponade with special attention paid to the volume and consistency of drainage in the collection chamber (D) (Fig. 3).
-
Allibone, L (2003) Nursing Management of chest drains. Nursing Standard, Vol.12 (17), pp. 45-54.
-
Allibone, L (2005) Principles for inserting and managing chest drains. Nursing Times, Vol. 101 (42), pp. 45-48.
-
Atrium (2016) A personal guide to managing chest drainage. Atrium teaching resource accessed at: http://www.atriummed.com/EN/chest_drainage/ocean.asp and http://www.atriummed.com/EN/Chest_Drainage/Documents/Ocean-BlueHandbook-010140.pdf
-
Balfour-Lynn, IM Abrahamson, E Cohen, G Hartley, J King, S Parikh, D Spencer, D Thomson, AH Urquhart, D (2005) BTS guidelines for the management of pleural infection in children. Thorax, Vol. 60, Suppl. I, pp. i1-i21.
-
Bar-El, Y Ross, A Kablawi, A Egenburg, S (2001) Potentially dangerous negative pressures generated by ordinary pleural drainage systems. Chest, Vol. 119 (2), pp 511-514
-
Briggs, D (2010) Nursing care and management of patients with intrapleural drains. Nursing Standard, Vol. 24 (21), pp. 47-55.
-
Coughlin, AM Parchinsky, C (2006) Go with the flow of chest tube therapy. Nursing, Vol. 36 (3), pp 36-41.
-
Crawford, D (2011) Care and management of a child with a chest drain. Nursing Children and Young People, Vol.23 (10), pp.27-33.
-
Day, TG Perring, RR Gofton, K (2008) Is manipulation of mediastinal chest drains useful or harmful after cardiac surgery? Interactive Cardiovascular and Thoracic Surgery, Vil. 7, pp 888-890.
-
Duncan, C Erikson R (1982) Pressures associated with chest tube stripping. Heart and Lung, Vol. 11 (2), pp. 166-171.
-
GOSH (2016) Chest drain management. Great Ormond Street Hospital: Clinical Guidelines, London.
-
Halm. MA (2007) To strip or not to strip? Physiological effects of chest tube manipulation. American Journal of Critical Care, Vol. 16 (6), pp. 609-612.
-
Havelock, T Teoh, R Laws,D Gleeson,F (2010) on behalf of the BTS Pleural Disease Guideline group. Pleural procedures and thoracic ultrasound: British Thoracic Society pleural disease guideline 2010, Thorax, Vol. 65 (Suppl.2), pp 61-76.
-
Horrox, F (2002) Chest drain management. In: Manual of Neonatal & Paediatric Heart Disease, Whurr, London.
-
Kwiatt, M Tarbox, A Seamon, MJ et al (2014) Thoracostomy tubes: A comprehensive review of complications and related topics. International Journal of Critical Illness and Injury Science, Vol. 4 92), pp. 143-155.
-
Lazzara, D (2002) Eliminate the air of mystery from chest tubes. Nursing, Vol.32 (6), pp 3643.
-
Maxwell, S (2015) Chest Drain Tutorial Notes. Paediatric Critical Care , Royal Hospital for Children, Glasgow
-
NHS Greater Glasgow & Clyde (2016) Infection Prevention and Control: Core prevention policies: Decontamination of Equipment and the Environment; Standard Precautions. NHS Greater Glasgow & Clyde Control of Infection Committee Policy. NHSGGC.
-
Scmelz, JO Johnson, D Norton, JM Andrews, M Gordon, PA (1999) Effects of position of chest drainage tube on volume drained and pressure. American Journal of Critical Care, Vol. 8 (5), pp. 319-323.
-
Shalli, S., Saeed, D., Fukamachi, K., Gillinov, M., Cohn, W.E., Perrault, L.P. & Boyle, E.D. (2009) “ Chest tube selection in cardiac and thoracic surgery: A survey of chest tube-related complications and their management”, Journal of Cardiac Surgery, Vol.24, pp.503-509
-
Sullivan, B (2008) Nursing management of patients with a chest drain. British Journal of Nursing, Vol. 17 (6), pp 388-393.
-
Thorn, M (2006) Chest drains: A practical guide. British Journal of Cardiac Nursing, Vol. 1 (4), pp 180-185.
-
Tooley, C (2002) The management and care of chest drains. Nursing Times, Vol. 98 (26), pp 48-50.
-
Wallen, M Morrison, A Gillies, D O’Riordan, E Bridge, C Stoddart, F (2007) Mediastinal chest drain clearance for cardiac surgery. The Cochrane Database of Systematic Reviews, Vol. 2, 2007.
Last reviewed: 30 September 2018
Next review: 30 September 2021
Author(s): Jeanette Grady
Approved By: PICU Clinical Guideline Group







