Home monitoring programme for children with hypoplastic left heart syndrome following Stage 1 Norwood or Hybrid Procedure
exp date isn't null, but text field is
Objectives
- Maximise morbidity-free survival of children with HLHS who have undergone a Norwood/Hybrid procedure, driven by reliable and regular contact with the Cardiac Nurse Specialist (CNS) team and Dietitian.
- Ensure early identification of potential complications which may require surgery or cardiac catheterisation.
- The purpose of this monitoring is not to deal with emergency situations if the patient acutely deteriorates at home. The normal procedure of dialling 999 and contacting Emergency Services should be followed.
Despite significant technical and management advancements improving the survival of children born with Hypoplastic Left Heart Syndrome (HLHS), patients with this condition remain at high risk of morbidity and mortality. The existing management strategy for HLHS typically includes an initial stage of palliation (the Norwood Procedure or Hybrid Procedure) which is followed by a second stage of surgical intervention (creation of the Bi-Directional Glenn). The time between these interventions - known as the inter-stage period - is a period of risk for children with HLHS. It carries a high risk of mortality.
The Home Monitoring Programme (HMP) was pioneered by the Children’s Hospital of Wisconsin because of this concern of high mortality between hospital discharge and the second stage of surgical management. Implementation of the HMP was based on the hypothesis that a drop in oxygen saturation from baseline, poor weight gain or weight loss may predict the presence of serious anatomic lesions or evolving illness and allow for life saving intervention. The introduction of this programme has been proven to reduce inter-stage mortality. This practice has been adopted in many centres with HLHS programmes in the USA, and increasingly the United Kingdom.
The Royal Hospital for Children (RHC) in Glasgow introduced a HMP for children with HLHS in 2011, with the shared aim of existing programmes in improving survival and reducing morbidity of infants with HLHS between first and second stage surgery. The discharge of infants with HLHS will be conditional upon fulfilling the discharge criteria dictated by the HMP; including optimised medication, optimised nutritional status and the demonstration of parental understanding and program compliance.
Principally this service will be delivered by the CNS Team and Paediatric Cardiology Dietetics, and supported where appropriate by:
- Consultant Paediatric Cardiologists/Registrars/Cardiac Advanced Nurse Practitioners.
- Ward 1E duty medical and nursing teams.
This protocol is applicable to every infant having undergone Stage 1 Norwood or Hybrid Procedure for HLHS with shunt or ductal stent-dependent pulmonary blood flow.
Any patient on the HMP who turns one year of age, will ordinarily cease being on the programme unless they remain shunt or stent dependent, and to remain on the programme, the named Cardiologist will need to request this.
The HMP criteria may no longer be applicable and suitable for patients over one year of age, and so this will need to be considered.
- Patient suitability for commencement on the HMP is decided by the patient’s named Consultant Cardiologist, and this decision is then to be communicated with the Cardiac Nurse Specialist (CNS) Service, Cardiac Dietitian, Ward Staff and the patient’s parents.
- Patients identified to commence on the HMP should be transferred appropriately to Ward 1E for training to be facilitated; if patient not already placed in 1E.
- HMP training is carried out by a Cardiac Nurse Specialist (CNS) and supported by ward staff.
- The patient is discharged home in possession of user-friendly baby weighing scales, an oxygen saturation monitor and a HMP patient diary containing call criteria.
- Parents are trained in all aspects of the HMP including how to use the equipment provided, how to document the infants HMP data within the diary and call criteria is explained.
- The medication, feeding and home monitoring plans (with specified weight, SaO2 and feed intake parameters) are signed off prior to discharge.
- The Paediatric Cardiology Dietitian will meet with the parents prior to discharge to discuss feeding and expected growth.
- There is a clear understanding of contact numbers and who to contact.
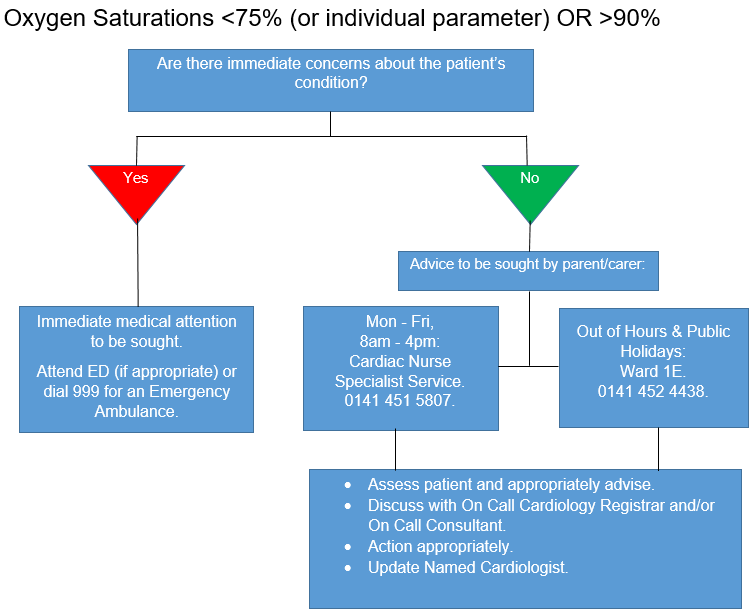
- Parents can contact the CNS Service Monday to Friday 8am-4pm on HMP phone 0141 451 5807.
- Outside office hours, calls are directed to Ward 1E.
- For feed/growth related questions parents will be given the contact number for the Paediatric Cardiology Dietitian.
- The CNS team contacts the Scottish Ambulance Service with patient’s details to be logged as a priority call out.
- The CNS team enrols the patient on the hospital’s Patient Alert System, identifying him/her as high risk and as a potential candidate for a capillary blood gas and lactate in the event of presentation to the Emergency Department.
- Prior to discharge home, the CNS team will check if the infant’s local hospital has a Patient Alert System that can identify the child as high risk. They will request that a message is logged advising that if admitted to A&E or hospital consideration should be given to performing a capillary blood gas and lactate and that the infants Cardiologist or the on-call Cardiologist are informed immediately.
- Discharge is approved only after the parents, Ward 1E nursing staff, CNS and Cardiologist are satisfied HMP training is complete and all discharge criteria met.
- Parents record the patient’s weight every day at the same time and before a feed.
- Parents spot check the patient’s saturation at the same time daily.
- The patient’s weight and saturation are logged in the Diary.
- Feeds volumes are documented in the Diary.
- There is at least weekly telephone contact with the CNS team and the Paediatric Cardiology Dietitian to review the diary and any concerns.
- Patient’s hydration is prioritised to assist in shunt protection.
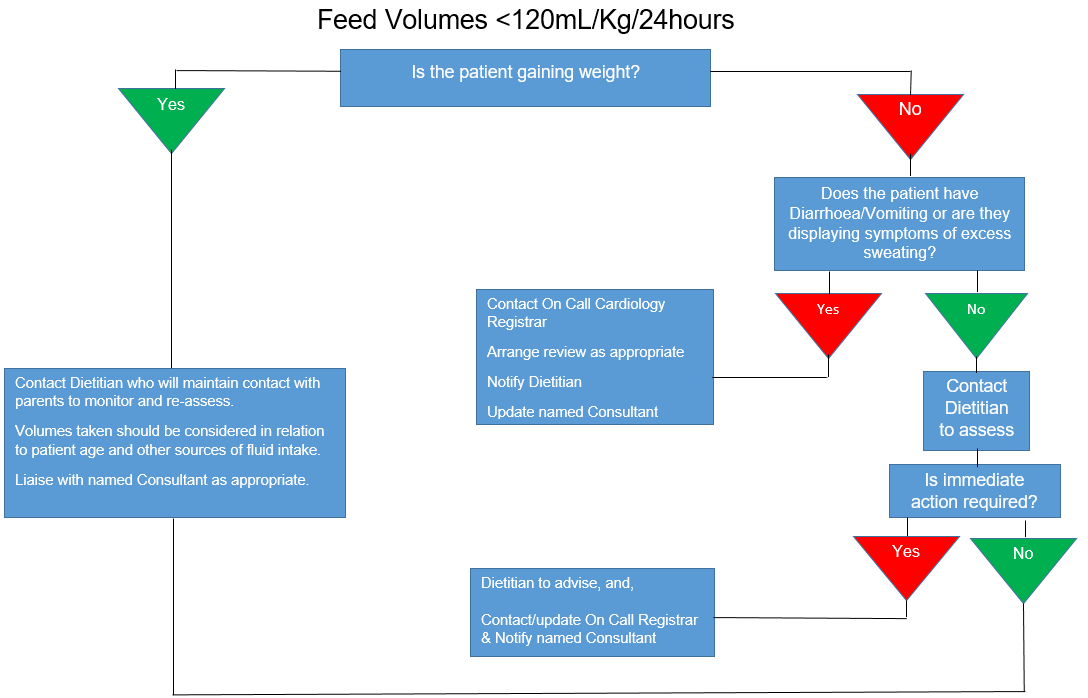
- If patient has a vomiting and diarrhoea illness the CNS team, Dietetics or Medical staff should be notified.
- Notification should also be given to the CNS team of any breach in agreed parameter limits or of any concerns as soon as possible.
- The CNS team are to be notified immediately, either by a parent or health care staff, if the patient presents for medical attention of any nature.
- Resting oxygen saturation drops below 75% (this may be modified following discussion with the named Cardiologist). Please see actions in Appendix A.
- Resting oxygen saturation is consistently above 90% (this may be modified following discussion with the named Cardiologist). Please see actions in Appendix A).
- Feed intake <120mL/kg/24hours (please see actions in Appendix B).
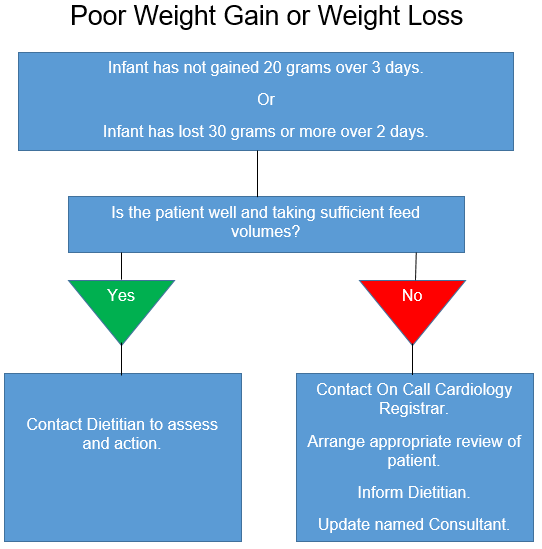
- The infant does not gain 20 grams over 3 days (please see actions in Appendix C).
- The infant loses 30 grams or more over 2 days (please see actions in Appendix C).
- Any concerns with the infants breathing pattern.
- Difficulty recording the infant’s oxygen saturations.
- If medical attention is sought, whether primary, secondary or tertiary level.
It must be remembered that each child will have an individually-prescribed set of normal parameters. It is critical that deviation from the norm for a particular patient be associated with a low threshold for early medical review.
In the first instance this may be at GP (if appropriate), Local Hospital, or RHC.
The Cardiologist, CNS Team and Paediatric Cardiology Dietitian are to be notified of A&E attendance immediately.
- Oxygen saturation, weight and feed intake data will be documented on Heartsuite.
- A weekly summary of the patient’s data will be added to Clinical Portal.
- Feeding Data are logged on Clinical Portal within Dietitian Notes.
- All parental calls for breach of parameter limits or general questions will be documented on Heartsuite and Clinical Portal.
- All HMP patients are followed routinely in a Cardiology Clinic and are seen when possible by the Consultant and CNS during each visit.
- HMP Diary reviewed in Clinic.
- Dietetics will review frequently by phone and attend clinics when possible.
CNS to update CNS team and Dietician on a weekly basis, which includes each HMP patient’s weekly data. Any concerns are highlighted.
The HMP MDT Team meet on a monthly basis as a channel of communication surrounding the HMP patients.
- Adherence to the HMP protocol will be assessed by regular review of patient data available on Heartsuite database and Clinical Portal.
- Audit of the HMP will occur regularly, including the administration of parental satisfaction questionnaires.
- The HMP protocol will be subject to formal annual review, which will be brought forward in the case of evidence to suggest earlier modification is needed.
- Any significant patient event will trigger review of the HMP as it pertains to that patient, to ensure the HMP objectives were achieved in that instance.
Azakie. T., Merklinger, S.l., McCrindle, B.W., VanArsdell, G.S., Lee. K.J., Benson, L.N., Coles, J.G., Williams, W.G. (2001) Evolving strategies and improving outcomes of the modified Norwood procedure: A 10-year single institution experience. Annals of Thoracic Surgery. Vol. 72(4):1349-1353.
Bridges, N.D., Jonas, R.A., Mayer, J.E., Flanagan, M.F., Keane, J.F., Castaneda, A.R. (1990) Bidirectional cavopulmonary anastamosis as interim palliation for high-risk Fontan candidates. Circulation. Vol. 82(suppl IV):IV-170-IV-176.
Carlo WF, Cnota JF, Dabal RJ, Ander-son JB. (2017) Practice trends over time in the care of infants with hypoplastic left heart syndrome: A report from the National Pediatric Cardiology Quality Improvement Collaborative. Congenital Heart Disease. Vol.12, Pages 315–321.
Crawford, R., Hughes, C., McFadden, S., Crawford, J. (2020) A systematic review examining the clinical and health-care outcomes for congenital heart disease patients using home monitoring programmes. Journal of Telemedicine and Telecare. Vol. 0(0), Pages 1-16.
Gaynor, J.W., Mahle, W.T., Cohen, M.I., Ittenbach, R.F., DeCampli, W.M., Stevens, J.M., Nicholson, S.C., Spray, T.L. (2002) Risk factors for mortality after the Norwood procedure. European Journal of Cardio-thoracic Surgery. Vol. 22:82-89.
Giglia, T.M., Stagg, A., Gardner, M. M., Natarajan, S., Ravishankar, C., Szwast, A.L., Jonathan, J., Rome, T. (2019) Interstage monitoring: Yes it makes a difference! Progress in Pediatric Cardiology. Vol. 54(1), 101140.
Kaplinski, M., Ittenbach, R.F., Hunt, ML., Stephan, D., Natarajan. S.S., Ravishankar, C., Giglia, T.M., Rychik, J., Rome, J.J., Mahle, M., Kennedy, A.T., Steven, J.M., Fuller, S.M., Nicolson, S.C., Spray, T.L., Gaynor, J.W., Mascio, C.E. (2020) Decreasing Interstage Mortality After the Norwood Procedure: A 30‐Year Experience. Journal of the American Heart Association. Vol. 9(19), e016889.
Mahle, W.T., Spray, T.L., Gaynor, J.W., Clark, B.J. (2001) Unexpected death after reconstructive surgery for hypoplastic left heart syndrome. Annals of Thoracic Surgery. Vol. 76:61-65.
Mahle, W.T., Spray, T.L., Wernovsky, G., Gaynor, J.W., Clark, B.J. (2000) Survival after reconstructive surgery for hypoplastic left heart syndrome: A 15-year experience from a single institution. Circulation. Vol. 120(suppl III): III-136-III141.
Metcalf, M.K., Rychik, J. (2020) Outcomes in Hypoplastic Left Heart Syndrome. Pediatric Clinics of North America. Vol. 67(5), Pages 945-962.
Nieves, J., Rudd, N.A., Dobrolet, N. (2018) Home surveillance monitoring for high risk congenital heart newborns: Improving outcomes after single ventricle palliation - why, how & results. Progress in Pediatric Cardiology. Vol.48, Pages 14-25.
Rudd, N.A., Ghanayem, N.S., Hill, G.D., Lambert, L.M., Mussatto, K.A., Nieves, J., Robinson, S., Shirali, G., Steltzer, M.M., Uzark, K., Pike, N.A., Vice Chair; on behalf of the American Heart Association Council on Cardiovascular and Stroke Nursing; Council on Lifelong Congenital Heart Disease and Heart Health in the Young; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Clinical Cardiology; and Council on Lifestyle and Cardiometabolic Health. (2020) Interstage Home Monitoring for Infants With Single Ventricle Heart Disease: Education and Management: A Scientific Statement From the American Heart Association. Journal of the American Heart Association. Vol. 9(16), e014548.
Tweddell, J.S., Hoffman, G.M.,Mussatto K.A., Fedderly, R.T., Berger, S., Jaquiss, R.D., Ghanayem, N.S., Frisbee, S.J., Litwin, S,B. (2002) Improved survival of patients undergoing palliation of hypoplastic left heart syndrome: Lessons learned form 115 consecutive patients. Circulation. Vol. 106(12) suppl I:182-189.
Last reviewed: 22 December 2023
Next review: 30 September 2026
Author(s): Lorraine Mulholland; Dr Ben Smith; Laura Flannagan
Approved By: Scottish Paediatric Cardiac Service

