Management of atopic eczema in children
Objectives
The aim of the guideline is to aid healthcare professionals involved in the management of eczema in children.
Scope
This guidance should be followed by healthcare professionals involved in the care of children with eczema.
Emollients should be prescribed for regular use in all eczema patients. They reduce the requirement for topical corticosteroids which should always be prescribed in addition.
Ointment based formulations (e.g. 50:50) are more effective at moisturising skin but creams (e.g. zerobase) are often preferred by patients for use during the day.
TCS should be applied to areas of eczema daily during flares and 2-3x per week for maintenance. The quantity required is indicated in the fingertip unit (FTU) guide (Table 1).
1 FTU is around 0.5grams of cream or ointment.

|
Number of (adult) fingertip units (FTU) |
|||||
|
Age |
Entire Face & neck |
Entire arm & hand (each) |
Entire leg & foot (each) |
Entire front of chest & abdomen |
Entire back & buttocks |
|
3-12m |
1 |
1 |
1.5 |
1 |
1.5 |
|
1-2yrs |
1.5 |
1.5 |
2 |
2 |
3 |
|
3-5yrs |
1.5 |
2 |
3 |
3 |
3.5 |
|
6-10yrs |
2 |
2.5 |
4.5 |
3.5 |
5 |
|
Over 10 yrs |
2.5 |
4 |
8 |
7 |
7 |
Table 1 – Fingertip units
- Generally ointments are preferable to creams, though creams are helpful in weepy areas.
- Parents should be instructed to leave 30 minutes between applying the emollient before applying the TCS.
- TCS should be applied once daily during acute flares of eczema. Potency & duration depends on severity of the flare (Table 2).
- Step-down of potency is required on the face as directed
- Maintenance treatment should be continued as directed unless skin is completely clear for 14 days. If eczema returns then treatment should be restarted.


*There have been ongoing issues with the availability of Clobetasone butyrate in the UK. An alternative TCS suitable for use on the face is Aclometasone dipropionate cream which is mild to moderate in potency if not infective. For use on the body Betamethasone valearate cream is very similar in potency to Clobetasone butyrate ointment.
Table 2 – Management of atopic eczema in children
Patient eczema management plan for discharge can be printed here: Eczema Management Plan - RHC Emergency Department
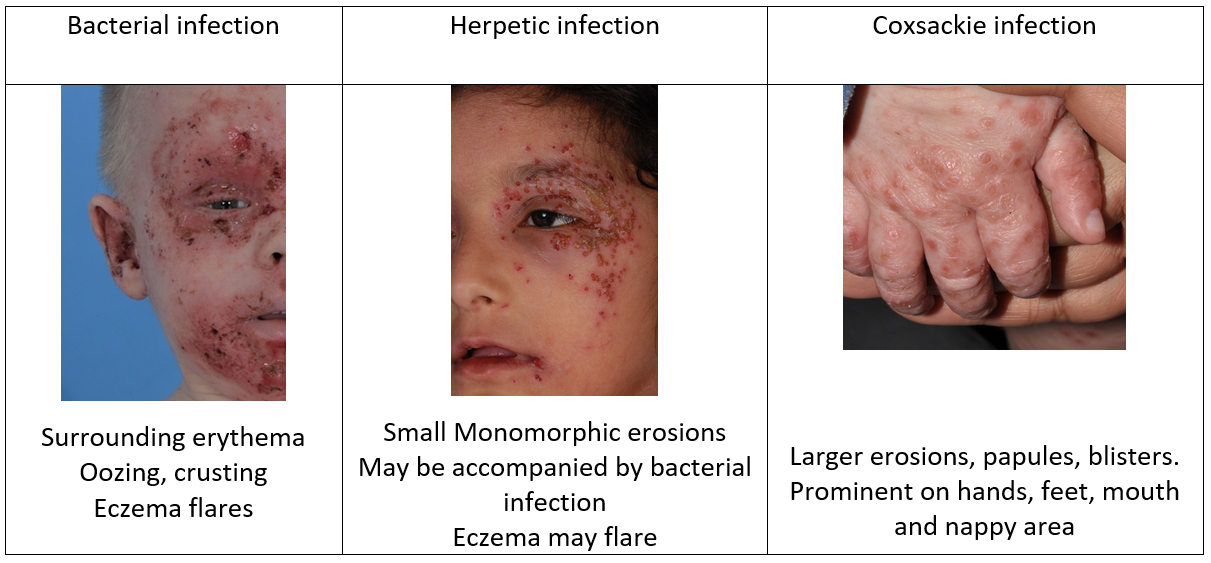
Atopic Eczema is associated with an impaired skin barrier. This leads to dryness and increased susceptibility to irritants, allergens and infection. People with atopic eczema carry S. aureus in about 90% of affected areas and the density of S. aureus increases with the severity of the eczema. Whilst carriage of S. aureus does not equate to infection, swabs from areas of erythema, crusting, weeping and oozing often produce heavy growth on culture and in these circumstances the bacteria contribute to exacerbation of the eczema.
It is therefore important to treat both the eczema and secondary infection in a child with infected atopic eczema. Infected eczema should not be managed with antibiotics alone as this does not manage the eczema flare, fails to restore the skin barrier and prolongs morbidity/duration of admission.
If the skin is clinically infected oral antibiotic or topical antimicrobial /antibiotic should be used in addition to the topical steroid.
Investigation
A Bacterial skin swab should always be taken before initiation of oral antibiotics.
If recurrent infections are reported the anterior nares should also be swabbed.
Viral skin swab should be taken if there are monomorphic erosions or recent herpetic infection in a relative.
Management of infected eczema
- Bathing - A bath emollient with an antiseptic additive such as Dermol 600® should be added to the bath water.
- Emollients - Ensure that the child does not use tubs of creams/ointments from home as may have become contaminated by S. aureus. Prescribe the child’s usual emollient to be applied 3-4 times daily. If the child’s skin is dry increase the greasiness to an ointment. Parents should be advised to transfer a small amount onto a saucer or piece of kitchen towel with a spatula/spoon (not hand) and throw out what is left when finished applying rather than putting back into the tub.
- Topical corticosteroids – see Table 2 for TCS choice & duration
- Managing bacterial infection - Protocol for managing bacterial skin infections as per GG&C guidelines with oral or IV antibiotic as indicated by clinical severity
- Managing herpetic infection
If accompanied by secondary bacterial infection, it is important that the viral and bacterial infection and the eczema flare are managed in tandem.
- Treat with oral or IV acyclovir as indicated by clinical severity.
- Urgent Ophthalmology review if near to eye.
- Once Aciclovir (+/- antibiotics if secondary bacterial infection is present) has been initiated (2 doses given) then eczema should be managed as per Table 2 including application of topical corticosteroids +/- antimicrobial to areas of eczema. Delay between Initiation of Aciclovir/Antibiotics and steroid application should not be more than two doses.
Indication for admission (admit under medical paediatrics with dermatology input)
- Disseminated eczema herpeticum or severe bacterial infection
- Severe eczema <12mths old with failure to thrive
- Welfare concerns e.g. caregivers unable to provide appropriate eczema treatments at home
Request for RHC Dermatology team review is available via Trakcare referral within normal working hours. Please call the dermatology secretary on 86596 to inform them following submission of the Trakcare form. Out of hours advice can be sought from GG&C on-call dermatology via switchboard if urgent.
Indications for outpatient dermatology referral
- Severe eczema any age
- Moderate eczema failing to respond to treatment with 1% Hydrocortisone strength to face and Eumovate strength applied o.d for 1 week, then twice weekly for maintenance, repeating the week of o.d treatment for flares (as per Referral pathway dermatology.nhs.scot) or repeated ED attendances
A referral can be made by dictated letter.
Last reviewed: 18 December 2023
Next review: 31 July 2025
Author(s): Dr Sarah McCusker (Specialty trainee in dermatology, QEUH, Glasgow); Dr Paula Beattie (Consultant in paediatric dermatology, RHCG); Dr Gillian Campbell ( Consultant in paediatric emergency medicine, RHCG)
Version: 2
Approved By: Paediatric Emergency Medicine Clinical Governance Group, RHCG
Document Id: 356

