Preoperative fasting of patients for theatre, Royal Hospital for Children
Objectives
This guideline aims to:
- Decrease the incidence of prolonged starvation in patients undergoing elective surgery at the Royal Hospital for Children.
- Increase patient and parental comfort and satisfaction as a result of minimised fasting times.
The risk of pulmonary aspiration must be balanced with the risk of discomfort, hunger, thirst, dehydration and hypoglycaemia. These guidelines are written in the context of recent national and international publications and recommendations (1).
Scope
This guideline is for all patients prior to surgery / general anaesthesia.
Patient exclusions from this protocol include children who require longer for gastric emptying to occur. Such patients may include:
- Critically ill children
- Renal failure
- Severe Gastro-oesophageal reflux disease (limiting growth)
- Enteropathies / active intra-abdominal pathology
- Oesophageal strictures/patients booked for oesophageal dilatation
- Achalasia
- Mitochondrial disease
- Patients undergoing emergency surgery*
If you have any doubts about the fasting times for a patient, please contact their anaesthetist. The anaesthetist can be identified from the weekly rota or by phoning theatre reception on 84344/84345.
*Fasting guidance for patients undergoing emergency surgery should be decided by the anaesthetist on-call for Theatre 6. Their suitability for this guidance will depend upon their surgical and clinical condition. The on-call anaesthetist can be contacted on:
- 0141 452 4342 / extension 84342 (Registrar)
- 0141 452 4343 / extension 84343 (Fellow/Senior Registrar)
- 0141 452 4378 / extension 84378 (Consultant)
Audience
This guideline is for use by all health professionals in the Royal Hospital for Children, Glasgow who are involved in preparing patients for surgery. Administrative staff involved with communicating with patients and carers prior to procedures should also be familiar with this guideline.
Patients undergo fasting to minimise the risk of aspiration of gastric contents under anaesthesia. Over-fasting, especially in neonates and young infants, can lead to hypoglycaemia, thirst, hunger, irritability and dehydration. This can reduce patient comfort and make building rapport or securing venous access more difficult. Patients and parents should actively be encouraged to maintain hydration up until the requested fasting time for clear fluids to minimise these side effects. Ensuring a child is adequately hydrated prior to a procedure is as important as correct fasting.Hydration with a glucose-containing juice should be strongly encouraged. Water should only be used if glucose-containing juice is refused.
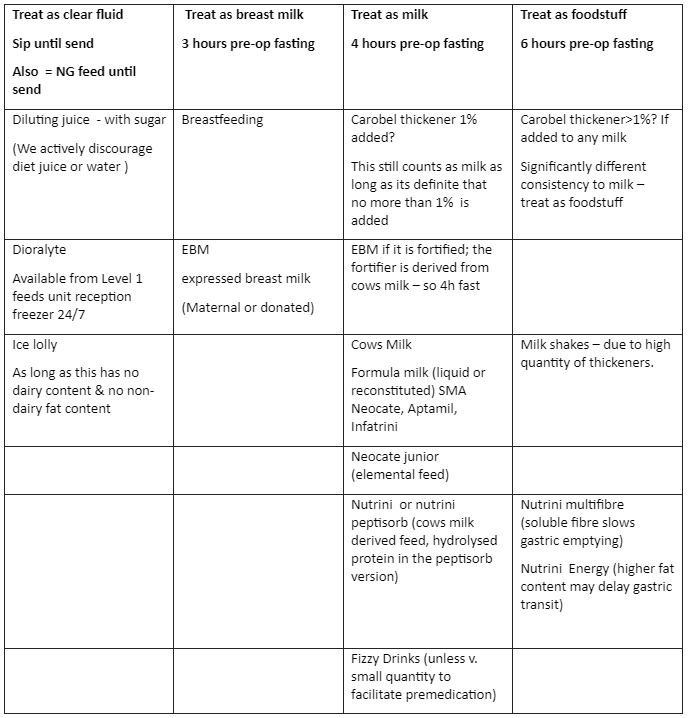
These guidelines balance the risk of aspiration with the risk of over-fasting. Children should be fasted for the minimum time possible. Although traditional guidance recommended 6 hours for solids, 4 hours for breast milk and 2 hours for clear fluids, recent evidence has shown that drinking clear fluids until 1 hour before surgery does not increase the risk of aspiration (2). Breast milk fasting times have been reduced to 3hours, and all other milk can be consumed up until 4 hours pre-operatively. Gastric content reduces exponentially after clear fluids with the median half-time less than 30min (3, 4). When glucose is included in the clear fluid, then gastric emptying is significantly quicker (2).
Clear fluids include water, diluting squash, ready diluted juice (e.g. Fruit Shoot®, Ribena®). Selected ice lollies are also allowed (not milk- or chocolate-based).
Clear fluids do not include milk, formula milk, pure fruit juice and fizzy drinks.
On admission to the Day Surgery Unit or ward, patients should be offered a clear drink or ice lolly of their choosing. An equivalent volume of ‘Slushie’ ice is also be permitted.
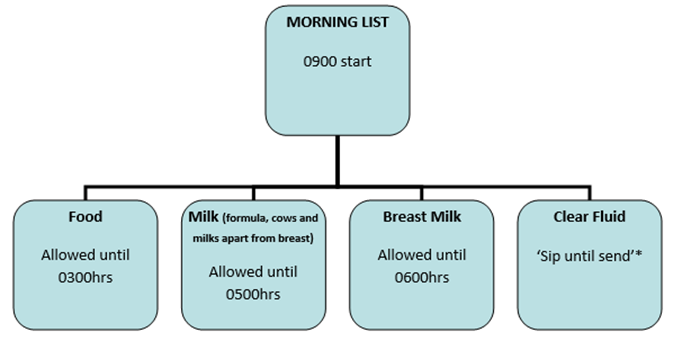
*’Sip until send’ means that sips of juice can continue up until the point that they are sent for. This is the default position of our hospital unless specific instructions are given otherwise by the anaesthetist. ‘Sip until send’ volumes should be explicitly limited to less than 5ml/kg.
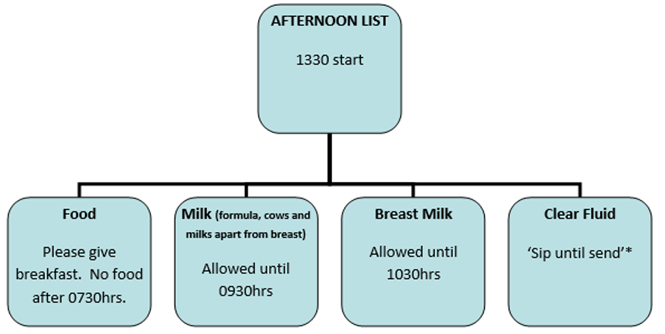
*’Sip until send’ means that sips of juice can continue up until the point that they are sent for. This is the default position of our hospital unless specific instructions are given otherwise by the anaesthetist. ‘Sip until send’ volumes should be explicitly limited to less than 5ml/kg.
Patients under the age of 18 months can be offered a few drops of 24% sucrose orally or onto a dummy to assist with pacification if required. The Oral Sucrose guidelines can be accessed here.
Chewing gum is regarded as requiring a 6 hour fasting time.
These are considered to be a food.
Families and staff should be given accurate and consistent information relating to fasting. Written guidance should be given to patients and parents when they attend pre-assessment clinic, and/or when their booking letter is sent out. The importance of providing food up until the fasting time (where practical) and clear fluids containing sugar until sending must be clearly explained to parents & guardians.
Trauma and acute illness can delay gastric emptying, and so fasting guidance for patients on the emergency list will be defined by the on call emergency anaesthetist. The running of the emergency list often changes throughout the day and the theatre staff must be mindful of avoiding unnecessary over-fasting of these patients “just in case” a slot becomes available. Patients with minor trauma (e.g. lip laceration, finger laceration) who will not be attending theatre imminently should be encouraged to drink clear fluids. If uncertain, contact the on-call team in theatre 6.
- Thomas M, Morrison C, Newton R, Schindler E. Consensus statement on clear fluids fasting for elective pediatric general anesthesia. Pediatric Anesthesia 2018;28:411-414.
- Kelly CJ, Walker RW. Perioperative pulmonary aspiration is infrequent and low risk in pediatric anesthetic practice. Pediatr Anesth. 2015;25:36-43
- Andersson H, Hellström PM, Frykholm P. Introducing the 6-4-0 fasting regimen and the incidence of prolonged preoperative fasting in children. Pediatr Anesth. 2018; 28 (1); 48-52
- Schmitz A, Kellenberger CJ, Liamlahi R, et al. Gastric emptying after overnight fasting and clear fluid intake: a prospective investigation using serial magnetic resonance imaging in healthy children. Br J Anaesth. 2011;107:425-429.
Last reviewed: 21 January 2024
Next review: 31 December 2026
Author(s): Alyson Walker, Consultant Paediatric Anaesthetist
Version: 2
Author Email(s): alyson.walker@ggc.scot.nhs.uk
Approved By: Paediatric & Neonatal Clinical Risk & Effectiveness Committee
Reviewer Name(s): Dr Graham Bell & Dr Dannie Seddon, Consultant Paediatric Anaesthetists
Document Id: 661

