Intermittent / borderline hyperglycaemia
exp date isn't null, but text field is
Objectives
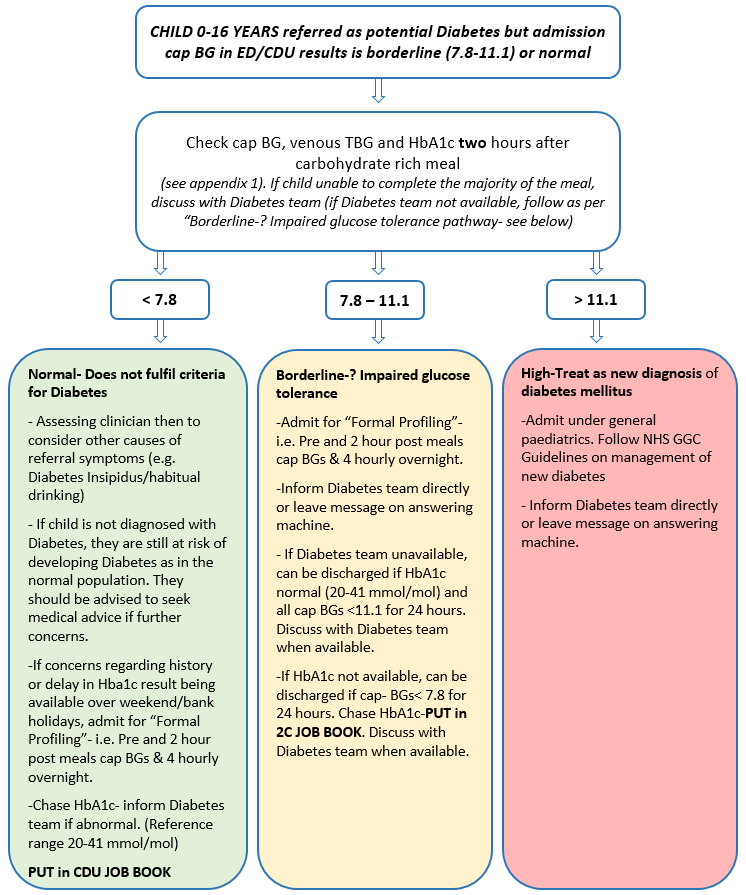
For acute medical staff in CDU and ED when assessing well children with intermittent/borderline hyperglycaemia where criteria is not met for Diabetes.
To guide how to manage children who have been referred for possible Diabetes but a repeat random capillary blood glucose (cap BG) in ED/CDU is in the borderline or normal range
In most cases the diagnosis of Diabetes is straightforward.
Child 0-16 years with symptoms of Diabetes and random venous blood glucose ≥ 11.1 mmol/l or fasting venous blood glucose ≥ 7 mmol/l (WHO criteria 2006/2011)
Treat as Diabetes - See “Walking Wounded” and “DKA” Guidelines
However, children may present with intermittent/borderline hyperglycaemia and glycosuria in the early stages of Type 1, as a presentation of Type 2 (increasing in incidence – especially in overweight adolescent population) or in monogenic diabetes. Hyperglycaemia may resolve after even a short period of fasting which often happens during referral to hospital.
In some cases, the child has simply not washed their hands (alcohol gel does not count).
Children with a previous high cap BG/ glycosuria/ clinical suspicion of diabetes who are discharged because repeat random cap BG is in normal or borderline range. This puts them at risk of the diagnosis being missed which may lead to them representing in DKA.
Please see Incidental hyperglycaemia/glycosuria for children who have an elevated glucose in association with illness/stress/medication.
Diabetes medical team - 0141 452 4961
Diabetes Hot nurse - 0141 452 4646
Out of Hours- General Paediatric team
These children are well, expected to have a normal appetite and are usually happy to be offered CHO rich options. Below are some suggestions for a CHO rich meal. The majority of these foods are available in CDU but patients may prefer alternatives that are brought by the parents.
Breakfast: Age appropriate portions of
- Cereal +/- toast/pancake
- Portion of fruit
- 1 x fruit juice or cup of milk
- 1 x yoghurt
Lunch/Tea: Age appropriate portions of
- Soup (optional)
- Bread or toast / sandwich / wrap / baguette / pasta salad
- Yoghurt / Rice Pudding / Custard
- Portion of fruit
- 1 x fruit Juice or cup of milk
- Cereal bar / pancake / Crisps / biscuit (optional if still hungry or if one of the other items is not eaten)
Last reviewed: 06 February 2024
Next review: 28 February 2027
Author(s): Karen Whyte
Author Email(s): Karen.whyte2@ggc.scot.nhs.uk
Approved By: Paediatric Guideline Group

