Hyperkalaemia: a guideline for management in neonates
exp date isn't null, but text field is
Objectives
This document outlines the management of newborn infants with high potassium levels >6.5 mmol/l. It is applicable to all medical, nursing and midwifery staff caring for the newborn in hospital. The guideline should be used with reference to the appropriate pharmacy monographs.
The normal range of serum potassium levels in the newborn is 3.5 – 6.0mmol/L. Hyperkalaemia is usually defined as a serum potassium level of >6.5 mmol/L. Hyperkalaemia is a potentially life-threatening condition, which if untreated can lead to fatal arrhythmias and death. It is most commonly seen in extreme preterm infants (<28 weeks) and/or very low birth weight (VLBW) infants (<1500g) including those without renal impairment (non-oliguric hyperkalaemia). Serum potassium levels in this population usually peak at around 24 hours of age. Proposed mechanisms for this include potassium release from catabolised cells, transcellular shift of potassium into the extracellular compartment and immaturity of renal tubular mechanisms responsible for potassium excretion. The onset of diuresis and increase in glomerular filtration rate facilitates potassium excretion and serum potassium levels usually normalise by 72-96 hours of age. This process may be complicated or delayed in certain pathologies which are important to consider if hyperkalaemia is detected. This guideline covers aetiology, diagnosis and acute management of hyperkalaemia on the neonatal unit.
Decreased renal potassium excretion
- Acute kidney injury (e.g. secondary to sepsis or hypoxic ischaemic encephalopathy)
- Chronic kidney disease
- Adrenal insufficiency (Addison’s disease, Congenital Adrenal Hyperplasia)
- Renal tubular acidosis
- Extreme prematurity
- Drugs e.g. ACE inhibitors, NSAIDS, Potassium sparing diuretics
Transcellular redistribution of potassium (intracellular → extracellular)
- Bleeding or haemolysis (IVH, cephalohaematoma)
- Cell necrosis (e.g. bowel ischaemia)
- Metabolic acidosis
- Drugs e.g. beta blockers, suxamethonium, digoxin
Excessive administration of potassium
- Oral or parenteral potassium supplementation
- Incorrect administration of potassium containing fluid
- Blood transfusion
- Infants who are at risk of hyperkalaemia (e.g. extreme preterm or VLBW infants) should have serum electrolyte levels taken early and at regular intervals
- Falsely elevated levels are commonly seen in haemolysed heel prick samples, samples with significant leucocytosis or thrombocytosis and ETDA contaminated samples
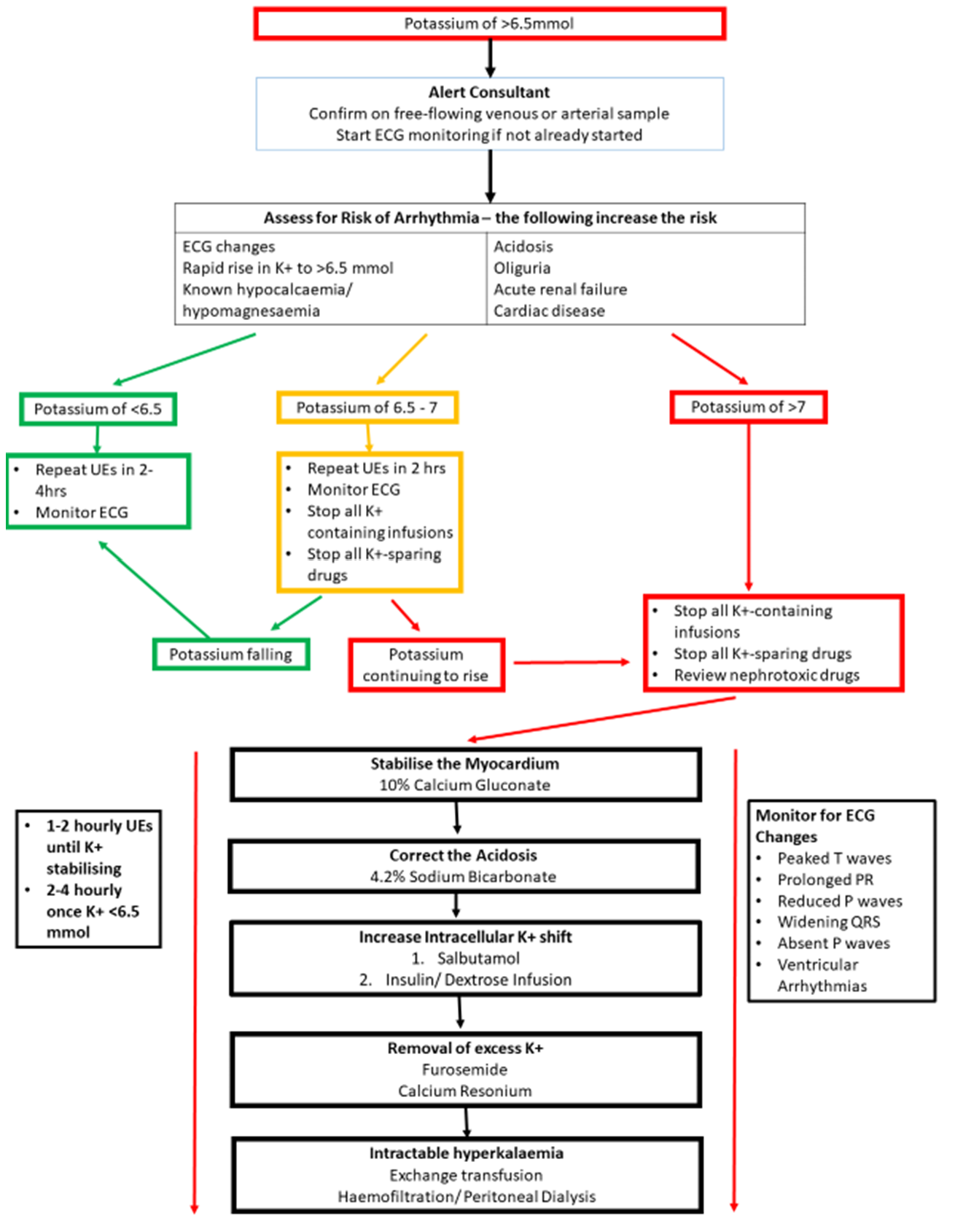
- If serum potassium is high (>6.5mmol/L) confirm with repeat free-flowing venous or arterial sample sent urgently to biochemistry and check immediate blood gas potassium with same sample
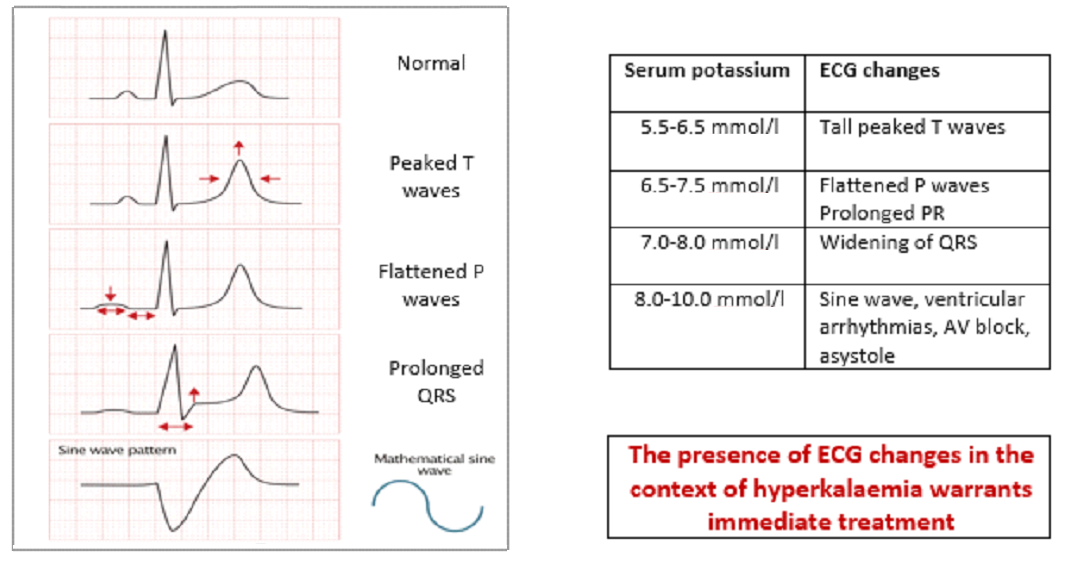
- Ensure continuous ECG monitoring is in place and review trace for associated changes (see below)
- Check urine output and assess for iatrogenic and/or pathological causes for hyperkalaemia
Cardiac arrhythmias:
- Hyperkalaemia can precipitate life threatening cardiac arrhythmias due to its effect on the resting membrane potential of the myocardium
- This can result in cardiac hyperexcitability → ventricular tachycardia/ventricular fibrillation or cardiac depression → bradycardia, AV block or asystole
- Ensure continuous ECG monitoring is in place for suspected or confirmed hyperkalaemia
- The presence of ECG changes (below) indicates myocardial involvement and warrants immediate treatment
- Consider a 12 lead ECG if interpretation is challenging but this should not delay treatment
- Note runs of tachycardia or bradycardia may indicate an impending arrhythmia
The reported mortality of neonates with hyperkalaemia is high even with treatment
* STOP ADMINISTRATION OF POTASSIUM IMMEDIATELY *
- Replace TPN with 0.18% saline +10% dextrose or 10% dextrose at maintenance rate
- Review Kardex and stop potassium-sparing and nephrotoxic drugs
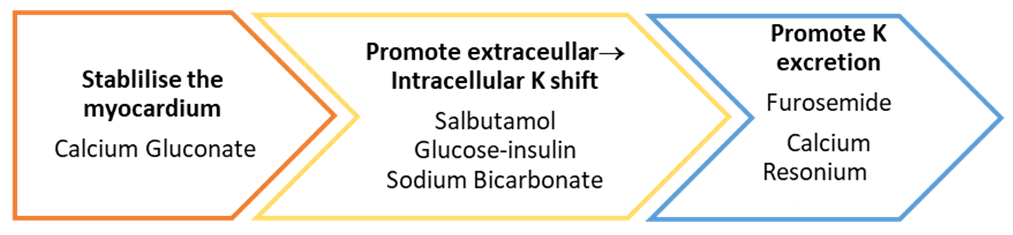
Flowchart for management of hyperkalaemia
*Refer to WOS or regional neonatal monograph for detailed guidance on dosage and administration (links to WOS monographs below)*
|
Drug |
Onset of action |
Monitoring/ |
Cautions and contraindications |
|
|
Within 5 mins |
Repeat dose if ECG changes persist after 10 mins Max total 3 doses Use ECG monitoring. Print or save rhythm for evidence |
Caution in patients on digoxin- run infusion over 30 mins Risk of extravasation *This will not reduce K+ concentration* |
|
Within 5 mins |
Should reduce K+ level by 1mmol/l Dose can be repeated after 2 hours |
Risk of tachycardia, hypertension and hyperglycaemia |
|
|
Within 15 mins |
Risk of hypoglycaemia- monitor blood glucose levels every 15-30mins for at least 6 hours after starting infusions Can repeat >30 mins after infusion stopped if potassium levels still raised >6.5mmol/l |
Stop if blood glucose <4mmol/l
|
|
|
Within 1 hour |
May be given even in absence of acidosis Equally as effective in Insulin/Dextrose |
Avoid if serum Calcium low- risk of worsening hypocalcaemia Not compatible with TPN solutions |
|
|
1-2 hours |
Monitor fluid balance |
Effect dependent upon adequate renal function Risk of ototoxicity with rapid administration |
|
|
1-2 hours |
|
Risk of intestinal haemorrhage and colonic necrosis Avoid in in the following groups: extreme preterm/VLBW neonates, those at risk of NEC, term infants with suspected bowel obstruction/ileus, recent GI surgery |
- U&Es should be checked hourly until potassium levels are starting to fall.
- They can be spread out to 2 hourly once this is the case.
- Once potassium is <6.5 mmol, U&Es can be checked 4-6 hourly.
In cases where the suspected cause of hyperkalaemia is due to an error in TPN preparation, this should be via the Suspected medicines defects guidance from the GG&C website.
Last reviewed: 01 January 2023
Next review: 01 January 2026
Author(s): Dr Andrew MacLaren – Consultant Neonatologist – Royal Hospital for Children, Glasgow; Dr Sharon Hodgson – ST5 Paediatric Trainee – West of Scotland
Co-Author(s): Other Professionals consulted: June Grant – Lead Clinical Pharmacist – Princess Royal Maternity Hospital, Glasgow; Anisa Patel – Senior Pharmacist – Royal Hospital for Children, Glasgow; Maria Tracey – Senior Pharmacist – Royal Alexandra Hospital, Paisley
Approved By: West of Scotland Neonatology Managed Clinical Network

