Phototherapy for neonatal jaundice
exp date isn't null, but text field is
Objectives
To provide clinical guidance on care of the baby receiving phototherapy which supports consistent delivery of family centred care practices across the Network. It includes the primary principles involved in treatment of jaundice in the neonate, maintaining the infants’ skin integrity, hydration, keeping the baby comfortable and clean and facilitating parental participation and bonding.
Audience
This guideline is applicable to all medical, nursing, midwifery and ancillary staff caring for neonates in the West of Scotland (WoS) in hospital and community settings. Staff should also be aware of the WoS Guidelines for Jaundice 1, hand hygiene and any relevant pharmacy monographs. Care of a baby receiving phototherapy will be approached with the aim of meeting the needs of the individual baby and family and the promotion of family centred care.
Neonatal Jaundice is the yellowing discolouration of the skin and sclera of a neonate, which is caused by increased levels of bilirubin in the blood. Neonatal jaundice is usually noted clinically when serum bilirubin is >85.5 micromol/L (5mg/dL) 2. Approximately 60% of term and 80% of preterm babies develop jaundice in the first week of life and approximately 10% of breastfed babies are still jaundiced at 1 month 3.
Most term babies have ‘physiological’ jaundice which may require a short period of phototherapy. However a few babies develop rapidly rising bilirubin levels which place them at risk of kernicterus. Any infant with high serum bilirubin or a rapidly rising bilirubin level needs to be treated urgently to avoid neurotoxicity 4.
Treatment for severe hyperbilirubinaemia includes phototherapy and/or exchange transfusion 2. The WoS Guideline on Neonatal Jaundice details the overall assessment and management of early and prolonged jaundice 1.
Phototherapy is universally recognised as the first option for the treatment of neonatal jaundice 5 and is widely used in neonatal units and postnatal wards. Phototherapy is a safe, effective method for decreasing or preventing the rise of serum unconjugated bilirubin levels and reduces the need for exchange transfusion in neonates.
Phototherapy involves the use of light waves to bring down bilirubin levels to normal through a process called photo-oxidation. Exposure to green-blue light at a wavelength of 420 - 550nm produces water-soluble isomers of bilirubin 6. This process facilitates dissolution of bilirubin in water by adding oxygen to it, which converts toxic bilirubin into water soluble non-toxic form and makes it easy for the liver to break it down, remove it out of blood and eventually excrete it in stool and urine.
The dose of phototherapy given largely determines how quickly it will work. The phototherapy dose is determined by the wavelength of the light, the intensity of the light, the distance between the light and the infant, and the body surface area exposed to the light. Appropriate management of jaundiced babies will enhance the effectiveness of phototherapy and minimise complications.
Phototherapy will normally be commenced if the serum bilirubin level is above the line for treatment when the result is plotted on a phototherapy treatment threshold graph 1. Factors such as the baby’s clinical condition, the presence of haemolysis, sepsis or hypoalbuminaemia may determine the need for treatment at a lower level than that indicated by the phototherapy chart. These cases will be referred to senior medical staff. Any baby who appears jaundiced should be assessed immediately as per the WoS Jaundice Guideline by use of a bilimeter if appropriate or a blood test; simple visual inspection is not reliable 1.
1. Conventional Phototherapy
In this type of phototherapy the baby is exposed to a specific type of light which looks blue but may emit light in the blue –green spectrum with wavelengths of 420-550nm This therapy is absorbed into the skin but doesn't damage the skin and may be required for several days. As this involves undressing the baby for maximum exposure of skin to light, the baby may have to be transferred to an incubator to maintain normal body temperature if not already in one.
Choice of incubator
An incubator that will be most conducive to effective phototherapy is one such as the Drager Babytherm 8000 (Figure 1) or the Weyer Thermocare, that have a relatively shallow hood. A shallow hood means that the phototherapy light can be placed closer to the baby thereby increasing the dose of phototherapy delivered.
The Giraffe Omnibed (Figure 2) and the Drager Isolette 8000 incubators have deeper hoods than the Babytherm but offer better thermoregulation and would be the incubator of choice for the smaller and / or preterm infant.
Figure 1

Phototherapy unit positioned correctly over a Babytherm 8000 incubator with baby lying on Biliblanket.
Figure 2

Giraffe Omnibed with single overhead neoBLUE phototherapy lamp
|
General Principles: Conventional Phototherapy |
|
Phototherapy is universally recognized as the first option for treating neonatal jaundice due to its efficiency and safety in reducing high serum bilirubin levels and limiting its neurotoxic effects. There are however, several studies which have suggested that phototherapy may elicit a series of short and long-term adverse reactions associated with paediatric diseases.5 These include:
- Overheating – monitor neonate’s temperature
- Water loss from increased peripheral blood flow and diarrhoea (if present)
- Diarrhoea from intestinal hypermotility
- Ileus (preterm infants)
- Rash
- Retinal damage
- ‘Bronzing’ of neonates with conjugated hyperbilirubinaemia
- Temporary lactose intolerance
The use of two or even three phototherapy units over an incubator has been applied when SBR/TBR levels are nearing exchange transfusion levels, rising exponentially or there is a risk of haemolysis. It has been reported that double phototherapy may reduce the duration of treatment however unclear if it reduces the need for exchange transfusion. Additionally the benefits of triple phototherapy compared to double is unclear 7.
A better option may be to place the baby in an incubator with a phototherapy unit on top whilst the baby lies with at least two thirds of his body on a Biliblanket. Multiple phototherapy units may mean that no one unit is positioned directly over the baby. If a Biliblanket is not available and two or more phototherapy light sources are required, then one phototherapy unit should be positioned directly over the baby with the others one angled to the side of the incubator.
Fibre-optic Phototherapy (Bilibed, Bilipad or Bilicocoon) is increasingly being used to treat neonatal jaundice in the term or near term baby. It provides a method of delivering safe and effective treatment while allowing better parental interaction/breastfeeding and improved parent satisfaction. It is recommended that conventional (overhead) phototherapy should only be used for babies who have or are suspected of having haemolytic jaundice (antibodies, DCT +ve, rapidly rising SBR or a very high SBR on initial presentation).
Bilibed
The Bilibed device is a fibre-optic phototherapy unit which can be fitted into the base of most standard Bassinettes (Figure 3a). This method can be used instead of overhead lights. The precisely directed light and the minimum distance from the baby ensure high light efficiency and therapeutic action. As it cannot be used within an incubator, or combined with overhead lights, it is recommended that use of the Bilibed should be limited to term or near-term infants with physiological jaundice who have no additional special care needs.
The fibre optic pad is designed to be placed within a disposable Bilisoft Cover and then correctly positioned underneath the baby ensuring the “brightest side “of the pad is next to the baby. This pad does not generate heat and will not interfere with the neonate’s thermal environment. Fibre-optic phototherapy limits the eye’s exposure to the phototherapy light but does not block this entirely. Therefore in accordance with the manufacturers’ instructions all neonates receiving phototherapy should have their eyes covered with opaque eye covers whenever phototherapy is administered.

Figure 3a - Bilibed in a Cot
Bilisoft Bilipad
The “Bilisoft” Bilipad is similar to the paddle in the Bilibed but does not have a rigid enclosure. This allows it to be used either in a bassinet or in an incubator. There are two pad sizes, for preterm and term infants. The Bilisoft Bilipad can be used on its own Figure 3b or combined with an overhead phototherapy unit to provide “double” phototherapy, as in Figure 1.
The BiliSoft Pad Covers and Pad Nests are specifically designed for use with the BiliSoft Phototherapy Systems, which are used to treat both premature and full-term infants for hyperbilirubinemia. The soft, cushioned, disposable BiliSoft covers are made of flame retardant, skin-friendly fabric. They are available in small and large sizes to match the size of the light pad. Materials used are engineered to allow therapy light to pass through the fabric and covers are x-ray compatible.

Figure 3b – Bilisoft BiliPad
Bilicocoon
The Bilicocoon phototherapy system has been designed to deliver controlled phototherapy to a greater proportion of the skin using either; a flexible nest which wraps around the baby; or a bag system which utilises two pads to treat the upper and lower surfaces simultaneously (figure 4). Its primary aim is to treat neonatal jaundice without compromising the relationship between mother and baby and facilitate parent–infant interaction and optimise breast feeding.
- Nest System
The nest system is reported as being more adapted for low birth weight or preterm babies. It consists of a large pad allowing wrapping and is adapted for kangaroo care and the incubator.
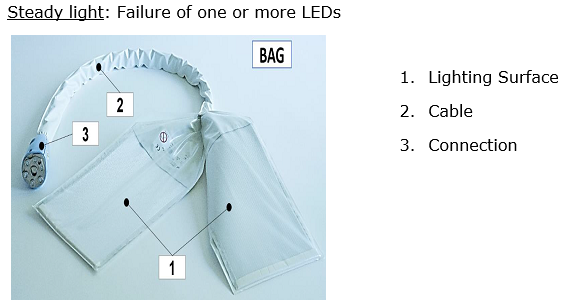
- Bag System
The bag system is reported as being more adapted for term babies. It emits light to front and back, providing 360° exposure. The bag system allows little light from escaping the bag and is adapted for handling, cuddling and breastfeeding the baby. The system is also available in a small size, called Small Bag, to offer a comfortable and effective solution for all different sizes of babies.
A demonstration of how to set up and work the Bilicocoon 8
Courtesy of Central Medical Supplies.
A SOP for the Bilicocoon can be viewed in Appendix 1.

Figure 4 Bilicocoon systems
It is important to include parents in the care of their baby when receiving phototherapy by explaining the need for and actions of phototherapy. This is particularly in relation to the need for the baby’s skin surface to be exposed to the phototherapy light and also the importance of keeping their baby warm when receiving phototherapy, maintaining a neutral thermal environment. Potential complications of phototherapy and the need for protective eye coverings during phototherapy treatment should be explained. The need for measuring the bilirubin level and need for blood sampling should also be explained. Parents should be told of the importance of keeping the baby under the light as much as possible but that this should not interfere with breastfeeding as a biliblanket / cocoon can generally be used.
Neonates receiving phototherapy (where there are no other contraindications) can have brief periods where the phototherapy is ceased so that they can be cuddled/breastfed and have their eye covers removed for parent-baby interaction to occur.
Phototherapy treatment for neonatal jaundice is generally undertaken in hospital. However, it is possible to safely administer home phototherapy (HPT) for jaundice in patients’ own homes 9,10. This practice is increasingly being accepted as an alternative to inpatient phototherapy for term neonates and helps to prevent prolonged hospitalisation and re-admission. It can promote mother–infant bonding and lead to increased parental satisfaction 11.
The Bilicocoon and Bilibed are a safe and easily adapted method of delivering phototherapy in the family home. Refer to local protocols for details of home phototherapy.
The Bilicocoon Phototherapy System is for the treatment of unconjugated hyperbilirubinemia in neonates and infants under 3 months old and weighing less than 10kg. Eye protection must be applied. Do not use on damaged skin.
Operation (image 1)

- On/Off
- Display’s hours left to run
- Increase/decrease hours & minutes for running time only works for 5 seconds after switch on
- Reset button to reset time, only available for 5 seconds after switch on
- Usage indicator : Steady blue light
Steady light: Treatment ongoing
Flashing blue light: Time set up but disconnected pad
Light is off: No treatment session on going or setup
- Overheating indicator
Steady light: Fan failure
Flashing light: Overheating of the light generator during treatment
- LED failure indicator
Equipment required
- Bilicocoon
- Disposable Bilicocoon mattress cover
- Eye protection
Set Up

- Apply Mattress cover please note that front of mattress is shorter side and this should have the patterned side of mattress cover
- Cocoon baby comfortably, using tabs to secure cover and help maintain good position in mattress and apply eye protection.
- Attach pad connection (3) to connection port, ensure that this is connected well, if any light emits from connection port when switch on this will reduce the about of phototherapy treatment the baby will receive.
- Power on
- Increase treatment time (if required) within the first 5 seconds after powering on by pressing (+3 image 1), if you increase to maximum setting 99.5 hours this will reduce the chance of phototherapy stopping prematurely.
- Treatment will commence within 5 seconds of setting the time. Check no light is showing around connection port.
- Check usage indicator has a continuous blue light, a flashing light highlights connection issue (5 on image 1)
- To discontinue use Power off
Cleaning
Lightbox
- Wait 5 minutes after switching Bilicocoon off before cleaning
- Unplug power cord and socket
- Clean with detergent or disinfectant wipe. Be careful not to let the cleaning agent infiltrate the light box. *Take care when cleaning the connection port to avoid damaging the optical lenses
- Check that lightbox is clean, if not repeat above steps and then dry.
Pad
- Disconnect from light box
- Wipe using disinfectant or detergent wipe - ensuring again all areas covered and making sure all debris removed, ensuring that all hard to reach areas are decontaminated. Process may require to be repeated. Taking care to avoid damaging optical fibre.
- Visual inspection and repeat process as required.
Disinfection
If requiring a deeper clean, (contact with infection, blood or body fluids) use a suitable disinfectant agent, please refer to GGC SOP for decontamination of equipment.
Allow to air dry thoroughly before use.
Pad covers are disposable, single patient use
Important: If any light is omitting from any other area of device rather that patient mattress, this can reduce treatment received by baby, so report to medical physics
- WoS Neonatal Guideline (2021). Jaundice: neonatal guideline-NHSGGC.
- BMJ (2020). Neonatal Jaundice-BMJ Best Practice. https://bestpractice.bmj.com/topics/en-gb/672. [Accessed May 10th 2022]
- NICE Guideline (2010). Jaundice in newborn babies under 28 days (CG98), (last updated October 2016)
- Mitra, S., Rennie, J. (2017) Neonatal jaundice: aetiology, diagnosis and treatment. British Journal of Hospital Medicine (Lond) 2:78 (12) 699-704.
- Juan Wang, Genxin Guo, Aimin Li, Wen‑Qi Cal and Xianwang Wang (2021). Challenges of phototherapy for neonatal hyperbilirubinemia. Experimental and Therapeutic Medicine 21: 231.
- Woodgate, P., Jardine, A. (2015) BMJ Clin Evid.Published online 2015 May 22. PMCID: PMC4440981
- Roberton N.R.C. 1992. Textbook of Neonatalogy. 2nd edition. Churchill Livingstone.
- NeoMedLight (2016). How to use the BiliCocoon Bag Phototherapy System. Available at: https://www.youtube.com/watch?v=hMaKro2KxR8. (Accessed : 31 May 2022).
- Chu L, Qiao J, Xu C. (2020) Home-Based phototherapy versus hospitalbased phototherapy for treatment of neonatal hyperbilirubinemia: a systematic review and meta-analysis. Clin Pediatr . 59: 588–95.
- Szucs K.A, Rosenman M.B. (2013) Family-centred, evidence-based phototherapy delivery. Pediatrics. 131: e1982–5.
- Malwade U.S., Jardine L.A. (2014). Home‐versus hospital‐based phototherapy for the treatment of non‐haemolytic jaundice in infants at more than 37 weeks' gestation. Cochrane Database of Systematic Reviews. 6:CD010212
Last reviewed: 05 September 2022
Next review: 01 September 2025
Author(s): L. Raeside, ANNP, Neonatal Unit, RHC, QEUH, Glasgow
Version: 1
Co-Author(s): Claire Dinning, Neonatal Nurse Educator, RHC&RAH, GG&C
Approved By: West of Scotland Neonatology Managed Clinical Network

