Peripheral arterial lines: insertion and care
exp date isn't null, but text field is
Objectives
This Guideline is applicable to all Medical and nursing staff working in neonatal units in the West of Scotland. Only a suitable trained and competent medical practitioner/ANNP should undertake arterial cannulation. Separate guidance is available for aseptic technique for procedures and for taking blood samples from an indwelling arterial catheter.
Staff should also be familiar with the use of equipment to which the arterial catheters will be connected, including: syringe driver; invasive blood pressure monitoring system; and blood sampling circuits. The use of these is covered in separate guidance
An indwelling peripheral arterial line may be used when:
- There is a requirement for frequent arterial blood gas monitoring
- Continuous monitoring of arterial blood pressure is required1.
Umbilical arterial lines should be sited in preference to peripheral arterial lines during the immediate newborn period unless contraindicated.
The decision to site a peripheral arterial line should be discussed with the attending neonatal consultant. The need for arterial lines should be reviewed on a daily basis on the consultant ward round.
Where time permits explain the procedure to the parents, including what the procedure involves, the reason for the procedure and the potential risks of the procedure.
Peripheral arterial catheters should be sited where there is good collateral circulation
Preferred sites:
- Radial artery.
- Posterior tibial artery2
REMEMBER: the ulnar artery may be used instead of the radial artery if access to the radial artery is problematic, but must be avoided if the radial artery has recently been cannulated (or where an attempt at cannulation has occurred). Use of the ulnar artery must be discussed with the receiving neonatal consultant and documented in the baby’s case notes.
Other sites should be avoided, except by agreement with the attending neonatal consultant.
Contraindications to peripheral arterial line insertion include:
Absolute contraindications3
- Inadequate collateral blood flow or recent cannulation of a collateral artery in that limb.
- Unsuccessful Allen’s test (evidence of inadequate collateral flow).
- Evidence of reduced limb perfusion.
- Evidence of localised skin infection.
- Limb malformation, bone fracture
Relative Contraindication
- Uncorrected coagulopathy
All arterial lines must be connected to a pressure monitoring system.
This allows invasive blood pressure monitoring and also provides a warning of disconnection or occlusion of the catheter.
The pressure monitor will be connected to a closed circuit blood sampling set.
The arterial pressure monitoring system and blood sampling line should be primed before use and calibrated.
Patency of the peripheral arterial line is maintained with an infusion of 0.45% sodium chloride for infusion with 1 unit of heparin per ml (known as hepsal). See WoS drug monograph for Heparin – Arterial lines. The Heparinised saline should be changed every 24 hours.
REMEMBER: No other fluids / medications are to be given via an arterial line
Choose the most appropriate artery to cannulate. If a radial artery is selected check that an ulnar artery is present and patent using Allen’s test (see below).
The Allen’s test is used to assess collateral blood flow to the hands, generally in preparation for a procedure that has the potential to disrupt blood flow in either the radial or the ulnar artery. These procedures include arterial puncture or cannulation. A negative Allen test means that the baby likely does not have an adequate dual blood supply to the hand, which will present a contraindication to the planned procedure or at least suggest that further evaluation is necessary.

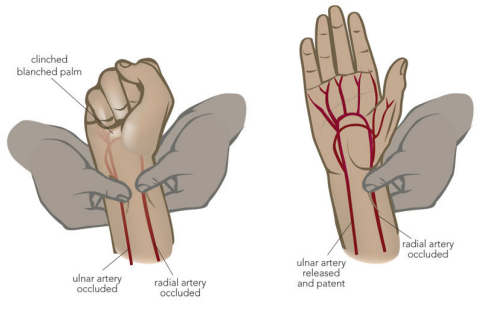
Procedure:
- Occlude both arteries at the wrist until the fingers appear blanched.
- Release the pressure on the ulnar artery.
- Observe the circulation returning to the hand, i.e. it will flush pink.
- If this does not happen within 7 seconds, do not proceed with a radial puncture on that side3.
When inserting a peripheral arterial line, a sterile procedure should be adopted in line with the applicable antisepsis guideline.
Preparation of Equipment
Prepare the following equipment on clean procedure trolley
- Dressing pack,
- 0.9% sodium chloride for injection (5mls),
- 2 ml syringe,
- 5ml syringe,
- 21G needles,
- Size 22G cannula
- 3 Way Tap, T – piece,
- Appropriate skin cleansing solution (refer to Antisepsis Guidelines),
- Transparent dressing,
- Splint
- Oral sucrose for pain relief if applicable – see oral sucrose guidelines
- Light for transillumination, if required.
REMEMBER: only cold light sources may be used - g. a Philips “Wee Site” or the Astodia “Diaphanoscope”
Insertion Procedure
- Wash hands and apply sterile gloves
- Flush the T-piece and 3 way tap with Sodium Chloride 0.9% IV solution
- Identify the vessel to be cannulated by palpation or transilluminate using a cold light source
- Perform Allen’s test to check for adequacy of collateral circulation
- Establish a sterile field around the cannulation site
- Cleanse the skin with appropriate cleansing solution (see separate guidance on asepsis for procedures). Leave for at least 30 seconds in order to allow the solution to dry
- Do not re-palpate the artery once the skin has been cleansed.
- Un-sheathe the cannula & hold it firmly so that the two component parts cannot become separated.
- Gently stretch the skin over the artery.
- Insert the cannula through the skin parallel to the vessel at a shallow angle. Advance the cannula slowly if the aim is to cannulate directly. An alternative approach is to advance quickly with the aim of transfixing the artery.
- If no flashback is seen, pull back slowly, as an artery may be transfixed. If so, a flashback may be seen as the cannula is withdrawn. When the flashback is seen try to advance the cannula over the needle to enter the artery. If no flashback is seen, pull the needle back to the level of the skin and redirect. If blood is seen in the cannula then remove fully and try again with a fresh cannula as it will be difficult or impossible to get a flashback with the original cannula.
- When the artery is punctured blood will be seen to fill the cannula rapidly. Sluggish back flow during an attempted arterial line cannulation may indicate either inadvertent venous cannulation or para-arterial placement, i.e. a haematoma.
- Decrease the angle of the cannula so that it is resting on the skin & try to advance the cannula over the needle and fully into the artery.
- Press firmly on the artery to occlude the blood flow, keep the cannula in position & withdraw the stylet.
- Continuing to protect the cannula, connect the T-piece, and 5ml syringe & flush with Sodium Chloride 0.9% IV solution (just sufficient to clear the cannula of blood).
- Check the site for skin blanching and swelling. If there is any evidence of compromised circulation at any point during the procedure, or after, consideration should be given to immediate removal.
- Connect to the arterial line set primed with heparinised saline.
- Secure the cannula with a sterile clear dressing. e.g. Tegaderm. Additional secure strapping of the tubing may be required to ensure adequate fixation.
- Apply an appropriate size splint but leave cannula visible for regular inspection. Radial lines should be splinted with the wrist extended. Ensure that all digits are clearly visible after securing the limb to the splint.
- Attach arterial line set to the transducer and monitor.
- Calibrate the transducer following the manufacturer’s instructions .
- Observe arterial trace on the monitor for appropriate waveform.
- Dispose of all equipment correctly as per Trust Policy
- Perform a social handwash.
- Document procedure in infants’ notes using the proforma sticker (Appendix 1) including:
- Date and time of insertion.
- Site of insertion.
- Indication for insertion of arterial line e.g. arterial blood gases.
- Cannula type and size.
- Any immediate complications.
- Indication of the quality e.g. sampling, flushing, good distal perfusion.
- Successful transducing.
- Signature, print name and grade.
Post-procedural care of the Cannula
Once successfully inserted, inspect the cannula site every hour and document findings on the observation chart. As these observations need to be made frequently staff should ensure that the site is easily visible and not covered with blankets or bedding.
If any concerns are identified they should be reported immediately to the medical staff
REMEMBER: Avoid inserting peripheral venous cannulae into the same hand or foot that has a peripheral arterial line in situ or that there has recently been an unsuccessful attempt at peripheral arterial cannulation until you are sure that perfusion to the limb is satisfactory.
Remove any unnecessary dressings which may impair clear viewing of the limb which contains a peripheral arterial line.
- Ensure the tubing and transducer are not pulling on the cannula.
- Inspect the area distal and proximal to the insertion site hourly for signs of:
- Compromised circulation: Cyanosis, blanching, delayed capillary refill time, decreased pulse, cool extremities.
- Displacement: bleeding, redness, swelling, fluid leakage, blanching, pain or discomfort, loss of arterial waveform on the monitor.
- Infection: Swelling, redness, exudate, pain, temperature change.
- Hourly observations of infusion rate, hourly volume infused, total volume infused, line pressure and review of line site.
- Never inject fluid boluses or medications into arterial line unless exceptional circumstances directed by the consultant.
Accidental displacement of the arterial cannula will require immediate application of pressure to the site for 5-15 mins or until bleeding has stopped.
The use of a guidewire (BabyWire ®) to site or reposition a peripheral arterial line should only be used under extreme circumstances and under the guidance of a Consultant Neonatologist. A guidewire should never be used in a preterm baby less than 34 weeks gestation.
Peripheral Arterial cannula should be removed when no longer required, or if there are complications or contraindications.
Procedure:
- Withdraw the cannula and apply pressure to the site with a piece of sterile gauze for 5 minutes. Ensure that the circulation to the hand or foot is maintained.
- Check to see if the bleeding has stopped if it hasn’t apply pressure for a further 2- 3 minutes before checking again. Continue until bleeding has ceased.
- Cover the site with a small piece of gauze and tape.
- Document that the arterial line has been removed in the infants’ record and on the observation chart.
- If an arterial line is removed because of concerns about the circulation distal to the insertion site, document this and highlight to ensure that future attempts at cannulation avoid the site. If perfusion does not return within a few minutes of removal this must be brought to the attention of the consultant medical staff.
- Vasospasm/thrombosis/thrombo-embolism which may lead to compromise of circulation, blanching, necrosis or gangrene of tissues or extremities 5 7
- Infection both local and systemic) 6 9
- Damage to peripheral nerves 3
- Haematoma/bleeding at the puncture site 3
- Extravasation
- Air Emboli 3
For management of a suspected arterial occlusion or thrombosis, see separate West of Scotland guideline on management of suspected arterial occlusion or thrombosis.
Continuous arterial blood pressure monitoring will be carried out on all babies with intra-arterial lines in situ. Arterial waveform analysis provides valuable information as well as the absolute systolic and diastolic pressures. The normal wave should have a sharp peak systole upstroke and a definite end diastole.
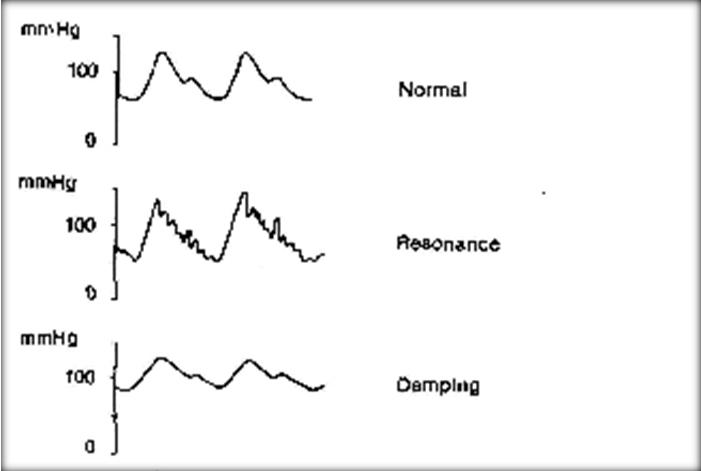
Diagram 2. Comparison of normal, resonant and damped arterial traces.
Maintenance: Calibration
The transducer must be zeroed:
- Following insertion of an arterial cannula
- At the beginning of every shift
- When transducer set is changed
During calibration it is essential that the transducer is level with the RIGHT ATRIUM so calibration should also be checked when the child’s position is changed4.
Recording
- The blood pressure is recorded continuously by the multi-parameter monitor which should have alarm limits set appropriate to the baby’s age and gestation
- The monitor should be set up to display the numerical values and arterial pressure trace
- Blood pressure should be recorded hourly on the baby’s clinical chart
- If the blood pressure is low and the arterial trace is dampened or lost, check all the tubing and connections for kinks, bubbles or disconnections. If all is in order, consider gently flushing the line and recalibrating the pressure transducer. If the problem persists then this should be reported to the medical staff
- Record hourly infusion of the heparinised 0.45% sodium chloride on the observation chart
- Gomella T.L. (2003) Percutaneous Arterial Catheterisation. In: Gomella T.L. Neonatology: Management, Procedures, On-Call Problems, Diseases and Drugs 5th Edition. McGraw-Hill Companies, pp 158-160.
- Halliday, H., McLure, G., Reid, M. (1998) Arterial Catheterisation. In: Halliday, H., McLure, G., Reid, M. Handbook of Neonatal Intensive Care 4th WB Saunders Company Ltd. p116.
- Safer Care Victoria (2021) Peripheral arterial access in neonates requiring intensive care [Accessed January 5 2023].
- Young, M., O’Boyle, C., Jaimovich, D.G. (1996) Pressure Transducers. In: Paediatric and Neonatal Transport Medicine. Mosby. pp 475-476.
- Hack WW, Vos A, Okken A. (1990) Incidence of forearm and hand ischaemia related to radial artery cannulation in newborn infants. Intensive Care Medicine. 16(1):503.[III]
- Furfaro S, Gauthier M, Lacroix J, Nadeau D, Lafleur L, Mathews S. (1991) Arterial catheter related infections in children. A 1year cohort analysis. American journal of Disease in Childhood. September;145 (9):103743. [III]
- Hack, W.W., Vos, A., Okken, A. (1990) Incidence of forearm and hand ischaemia related to radial artery cannulation in newborn infants. Intensive Care Medicine. 16(1):503.[III]
- Mense, L., Rose, S., Bruck, A., Rüdiger, M., Kaufmann, M., Seipolt, B. (2022) Peripheral Arterial Lines in Extremely Preterm Neonates. A Potential Alternative to Umbilical Arterial Catheters. Advances in Neonatal Care. Volume 22, Issue 4, p 357-361.
- Pratt RJ, Pellowe CM, Wilson JA, Loveday HP, Harper PJ, Jones SR, McDougall C, Wilcox MH (2007) epic2: National evidence-based guidelines for preventing healthcare associated infections in NHS hospitals in England. J Hosp Infect 65 Suppl 1: S1-64.
Last reviewed: 09 October 2023
Next review: 09 October 2026
Author(s): L. Raeside – ANNP, NICU, RHC, QEUH Glasgow; Dr A MacLaren – Consultant Neonatologist, RHC, Glasgow
Approved By: WoS Neonatology MCN

