Thermal care of the neonate
exp date isn't null, but text field is
Objectives
This guideline is applicable to all Midwifery, Nursing and Medical staff in The West of Scotland. The purpose of this guideline is to facilitate optimum thermal control in babies, potentially reducing the need for admission to the neonatal unit due to hypothermia.
SIGNS & SYMPTOMS OF HYPOTHERMIA
- Increased metabolism o Hypoglycaemia, Metabolic Acidosis, Hypoxia
- Increased pulmonary artery pressure o Respiratory distress, Tachypnoea
- Peripheral vasoconstriction o Acrocyanosis, cool extremities, decreased peripheral perfusion
- CNS depression o Poor feeding, apnoea, bradycardia, lethargy,
- Chronic Signs o Poor weight gain or weight loss
SIGNS & SYMPTOMS OF HYPERTHERMIA (Pyrexia)
- Tachycardia, Tachypnoea,
- Flushed appearance
- Lethargic
- Hypotonic
DEFINITIONS:
|
Normal temperature |
36.5º C to 37.5º C |
|
Hypothermia |
< 36.5º C |
|
Severe hypothermia |
< 32.0º C |
|
Hyperthermia |
> 37.5º C |
The term hypothermia refers to low body temperature. The neonates’ ability to maintain a normal body temperature may be impaired by environmental changes. Heat conservation is also impaired by the neonates’ large surface area to weight ratio, in addition low birth weight babies have less subcutaneous fat and less brown fat which is a source of heat production by non-shivering thermogenesis.
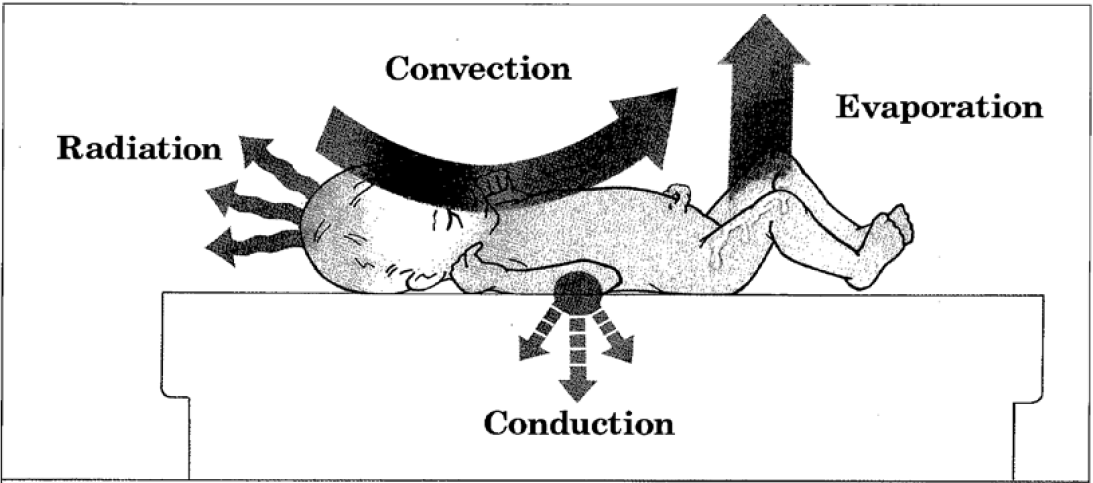
The neonate loses heat by:
- Convection (warm air is replaced with cold air by air currents around the baby)
- Conduction (baby comes into contact with cold objects)
- Evaporation (loss of heat when water evaporates from the skin or respiratory tract)
- Radiation (heat loss to colder surrounding solid objects not in direct contact with the skin).
Figure 1
Infants should be nursed in a neutral thermal environment and have a core body temperature between 36.5 – 37.5 degrees Celsius.
A neutral thermal environment is a temperature range within which heat production is at the minimum needed to maintain normal body temperature.
Heat production requires oxygen consumption and glucose use, persistent hypothermia can result in depletion of these stores, leading to metabolic acidosis, hypoglycaemia, decreased surfactant production, increased caloric requirements, and if chronic, impaired weight gain.
- Adequate environmental temperature in delivery room >25°C
- Ensure doors and windows are closed
- Ensure fans are switched off
- Pre-warm towels
- Hat available
1. The Well Term Baby
Immediate care
- Dry baby and remove wet towel
- Apply hat
- Skin to skin contact with mum
- Cover exposed skin with warm towel
- Initiate breast feeding
- Record temperature within first hour post delivery
- Delay bathing until temperature being maintained
On going care
- Temperature should be recorded daily preferably in the morning. If temperature below 36.5°C see Appendix A.
- Position cots away from outside walls and draughts
- Dress and wrap baby appropriately for environmental conditions
Late Pre-term babies on Postnatal Wards
There may also be babies being cared for in the postnatal wards who are less than 37 completed weeks gestation. These babies are at a greater risk of becoming hypothermic.
- For the first 48 hours these babies should have their temperature checked 4 hourly and then twice daily for the next 48 hours.
- Parents should also be advised not to bath the baby for at least the first 48 hours until temperature is stable.
- Dress baby appropriately. If baby’s temperature <36.5°C consider adding hat, cardigan and add more blankets. Check blood sugar to rule out hypoglycaemia.
- Skin-to-skin may also be used to increase the baby’s temperature as long as it is in a warm room and the baby is not exposed.
- Some units may introduce a NEWS (Neonatal Early Warning Signs) chart in the postnatal wards to monitor late pre-termers.
- If temperature remains low despite measures being taken to increase baby’s temperature then baby should be reviewed by medical staff.
2. Term Baby Requiring Resuscitation
- Place resuscitation table away from doors or draughts
- Ensure radiant overhead heater is on pre-warm
- Dry the baby with pre-warmed towels
- Remove wet linen and replace with clean dry linen
- Put on hat
- Baby should be on a non-conductive surface such as a mattress or dry towel under a radiant warmer
3. Preterm Baby (< 32 weeks gestation)
- Place resuscitation table away from doors or draughts
- Ensure radiant overhead heater is on pre-warm
- Deliver the baby feet first into a plastic bag (as per unit policy) covering the baby to the level of the neck, tucking around to seal.
- Dry the face and head and put on a good fitting hat
- Place the baby under the radiant warmer, do not cover with blanket
- If access is required to place lines or probes, pierce the bag at appropriate site. Do not unwrap the bag to expose the baby.
Please note following an URGENT FIELD SAFETY NOTICE use of Transwarmers with other heat producing devices such as radiant warmers and incubators is prohibited. Consideration should be given to using a heated mattress where the temperature can be controlled such as the Cosytherm mattress during procedures.
4. Transfer of Babies to Neonatal Unit
- When transferring babies from labour ward to neonatal unit using the transport incubator temperature of incubator should be at 37°C.
- Heated towels should already be in incubator
- If using a cot to transport the baby. Baby should be well wrapped and a hat applied. This principle should also be applied when transferring babies from labour ward to post natal wards.
5. Babies nursed/observed under radiant warmers
- Take temperature on admission and then 30 minutes after they have been placed under radiant warmer.
- Attach servo control probe to upper right quadrant of abdomen or whichever surface is closest to the radiant source.
- Ensure radiant warmer is switched to baby mode/servo and appropriate alarm limit set.
- The probe should be attached firmly to the skin with a reflective disc and disc should be visible at all times.
- Temperature of radiant warmer, skin temperature and axilla temperature should be recorded hourly.
- Baby should only have a nappy on, no clothes, except for a hat, and no blankets
- When a baby is nursed under a radiant warmer long term there will be an increase in insensible water loss. The use of bubble wrap will reduce insensible water loss and prevent heat loss to the environment.
6. Thermal care of a baby nursed in incubator
- All babies born at < 32 weeks gestation and/or <1500g should be nursed in an incubator initially.
- Axilla temp should be taken on admission.
- Choice of temperature monitoring
- Servo Control
- Skin Temperature
- Core-Peripheral Gap
- Whichever mode of temperature monitoring is used, temperature should always be continuously monitored. Upper and lower limits must be preset, with audible alarm set to activate if temperature is out with set limits.
Servo Control
- If using servo control this has been shown only to be effective in the first 14 days of life and should then be discontinued. Once servo control has stopped another mode of continuous alarmed monitoring should be commenced as necessary.
- When attaching a skin probe it should be attached to the upper right quadrant of the abdomen. Babies should never be nursed lying on the probe and the probe should never be covered with clothing or a nappy as this can give a falsely high temperature.
- The incubator skin temperature should be set initially between 36°C and 36.6 °C. The range of skin temperature for a preterm baby can be between 36.2°C and 37.2°C. Nursing staff should be aware that there will be a difference between the skin temperature and axilla temperature usually 0.5°C to 1.0°C. After a baseline skin temperature has been established the upper alarm limit may be increased to a maximum of 37.5°C if this is correlating with axilla temperature.
Skin Temperature
- If temperature is being monitored by a skin probe and incubator temperature being adjusted manually the skin probe must be attached to a central monitoring system which has alarm limits set.
- Incubator temperature should be adjusted by increments of 0.5°C if axilla temperature is above or below normal limits. If any adjustment is made to incubator temperature axilla temperature should be rechecked after 30 minutes. If no change in temperature, repeat above process.
- When attaching skin probe it should be attached to the upper right quadrant of the abdomen. Babies should never be nursed lying on the probe. The probe should not be covered with clothing or a nappy as this can give a falsely high reading. Alarm limits on central monitoring system should be set as for servo control mode.
Core-Peripheral Gap
- Core-peripheral gap is the difference between central and peripheral temperature.
- If the baby is exposed to cold stress, peripheral parts of the body will cool before there is a drop in the baby’s central temperature.
- The central-peripheral temperature difference (core-peripheral gap) increases as the baby is exposed to a cold stress and the peripheries cool. When the baby can no longer compensate by mobilising thermoregulatory mechanisms the central temperature drops.
- Measurement of the core-peripheral gap will give an early indication of thermal stress, long before there is any alteration in the central temperature.
- The axilla and the upper right quadrant of the abdomen (over the area of the liver) are alternative sites commonly used to represent central (core) temperature.
- Peripheral temperature is usually measured by a probe attached to the sole of the foot or the calf in extremely preterm infants.
- Both temperatures should be continuously monitored and displayed as a continuous trend, with alarm limits set.
- In babies less than 1000g the mean core-peripheral gap has been shown to increase from 0.5 degree Celsius on day 1, to 1 degree Celsius on day 3.
- In larger babies the core-peripheral gap has been shown to range from 1.0 to 1.3 degrees Celsius.
Data suggests that:
- A core-peripheral gap of around 1 degree Celsius is appropriate from day 3 of life but a gap of < 2 is considered within normal limits ̊
- The environmental temperature should be adjusted to maintain this value at 1.0 degree Celsius.
- A change in trend should alert the clinician to review baby
An increase in core-peripheral gap:
- Usually is due to cold stress
- May be due to hypovolaemia if there is an associated fall in blood pressure or rise in heart rate
- May be an early indicator of sepsis
7. Incubator Humidity
All babies born at less than 30 weeks gestation should be nursed in incubator humidity.
Premature babies are at greater risk of transepidermal water loss through evaporation. Incubator humidity can help reduce this risk.
- Babies born at < 28 weeks gestation.
Commence humidity at 80% (This may be difficult to achieve due to excessive rain out. If this is the case try to achieve at least 70%)
Continue on 80% for first 7 days
On day 8 wean by 5% daily
Stop humidity when you reach 40% as this is normal room humidity. - Babies born at 28 weeks to 30 weeks gestation.
Commence humidity at 80% (Again this may be difficult to achieve due to excessive rain out. If this is the case try to achieve at least 70%)
Remain at 80% until the end of day 1
On day 2 wean incubator humidity by 5% daily
Stop humidity when you reach 40% as this is normal room humidity.
Check axilla temperature within 1 hour of stopping incubator humidity and adjust incubator temperature as required.
When nursing a baby in humidity only open incubator portholes when necessary. If excessive rainout occurs clean inside of incubator. Increase room temperature and try to avoid having incubator directly under air vents.
When a baby is nursed in incubator humidity it may be necessary to change bed linen more often as it may get damp.
Incubator humidity boxes may be topped up throughout the day but emptied once completely in 24 hours and dried to reduce the build of a bacterial film. Distilled sterile water should be used for this process.
When humidity is stopped the humidity box should be removed and cleaned appropriately.
8. Respiratory Support
When a baby requires respiratory support via a ventilator or CPAP machine the gas which the baby receives from these machines is humidified via a separate humidifier. If this humidifier is not switched on then cold air is being delivered to the baby and this can cause hypothermia. When a baby commences respiratory support or the type of respiratory support is changed, two members of staff must check that the humidifier has been turned on and is at the required temperature. This should then be documented in the nursing charts that this has been carried out and signed by two members of staff.
9. Transfer from Incubator Care to Cot Care
Many factors need to be considered when changing a baby from incubator care to cot care.
- Infants Weight
Are they > 1500g
Have they regained their birth weight
Do they have a consistent weight gain - Incubator Settings
Incubator in Air Mode
Incubator temp 30°C or less
Axilla temperature 36.5°Cto 37.5°C - Physiologically Stable
No apnoeas, bradycardias requiring stimulation
If after considering the above factors the baby is fit to be transferred to a cot the following procedure should be followed.
- Prior to transfer dress baby with well fitting vest, sleepsuit, cardigan and hat. Preferably these clothes should be warmed in the incubator before dressing the baby.
- When transferred into cot cover with sheet and 2 blankets doubled over.
- Once transferred axilla temp should be checked hourly for the first 4 hours.
- If within this time axilla temp is 36.2°C to 36.5°C then consider transferring to a heated mattress.
- If axilla temperature less than 36.2°C then return to incubator.
- If after 4 hours axilla temperature is within normal range then recheck axilla temperature 4 hourly for the next 48 hours. After which time follow local protocol for checking axilla temperature.
If the baby needs to be transferred to a heated mattress this should be initially set to 37°C and axilla temperature checked within the first hour. Mattress temperature can be adjusted accordingly. Mattress temperature should be adjusted by 0.5°C and axilla temperature checked 3 to 4 hourly. Once the mattress temperature reaches 34°C and the baby maintains temperature within normal limits for 24 hours the baby should then be retried in a normal cot. Again check axilla temperature hourly for first 4 hours and follow above instructions.
10. Thermal Care for Babies Receiving Phototherapy in Postnatal Wards
Phototherapy can be delivered by several different methods and it is necessary to check the baby’s temperatures at regular intervals. Axilla temperature should be checked and recorded 30 minutes after phototherapy has commenced and then hourly for the next 4 hours. If temperature has been stable axilla temperature should then be checked and recorded every 4 hours until phototherapy stops.
When phototherapy has been stopped temperature should be checked after 30 minutes. If temperature within normal limits check again after another hour and if remains within normal limits baby can return to normal postnatal care ( see care of well term baby).

Allen K (2011) Neonatal thermal care: A discussion of two incubator modes for optimising thermoregulation.. A care study. Journal of Neonatal Nursing 17 43-48
Costeloe K, Hennessay E, Gibson AT, Marlow N, Wilkinson AR (2000) The EPICure Study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatrics 106 659-671
Freer Y, Lyon A (2012) Temperature monitoring and control in the new born baby. Paediatrics and Child Health 22(4) 127-130
Friedrichs J, Staffileno BA, Fogg L, Jegier B, Hunter R, Portugal D, Saunders JK, Penner JL, Peashey JM (2013) Axillary Temperatures in Full-Term Newborn Infants. Advances in Neonatal Care Vol 13, No 5 361-368
Horns KM (2002) Comparison of Two Microenvironments and Nurse Caregiving on Thermal Stability of ELBW Infants. Advances in Neonatal Care Vol 3 No 2(June) 149-160
Knobel R, Holditch_Davis D (2007) Thermoregulation and Heat Loss Prevention After Birth and During Neonatal Intensive-Care Unit Stabilisation of Extremely Low-Birthweight Infants. Advances in Neonatal Care. Vol. 10, No. 5S 7-14
Lyons A (2008) Temperature control in the neonate. Paediatrics and Child Health 18(4) 155-160
Lyon AJ, Pikaar ME, Badger P, McIntosh N. (1997) Temperature control in very low birthweight infants during first five days of life.” Arch Dis Child Fetal Neonatal Ed 76:F47-F50
Lyon AJ, Stenson B (2004) Cold comfort for babies. Archives of Disease in Chidhood Fetal and Neonatal Edition 89(1) 93-94
Sinclair JC. (1995) “Thermal environment, mortality and morbidity, state of the evidence.” In Okken A, Koch J (eds). Thermoregulation of the sick and low birthweight neonates. Springer-Verlag, Berlin.
Smith J, Alcock G, Usher K (2013) Temperature Measurement in the Preterm and Term Neonate: A Review of the Literature. Neonatal Network Vol 32 No 1 16-25
Waldron S, Mckinnon R (2007) Neonatal thermoregulation. Infant Vol 3 Issue 3 101-103
Last reviewed: 20 March 2023
Next review: 01 March 2026
Author(s): Sharon Lynch – Nurse Educator – Princess Royal Maternity, Glasgow; Lynne Raeside – ANNP – RHC, Glasgow
Co-Author(s): Other specialists Consulted: Marjorie Clarke – Senior Charge Nurse – Princess Royal Maternity, Glasgow
Approved By: West of Scotland Neonatology MCN
Document Id: 970

