Craniofacial SOP- PICU
exp date isn't null, but text field is
Objectives
This SOP covers the initial management of children that have recently undergone craniofacial surgery.
Scope
Post-operative craniofacial surgery patients.
Audience
Paediatric critical care staff.
Admit patient under Mr Koppel/ Mr Sangra
The majority of craniofacial cases will be extubated in recovery and will be admitted to a critical care setting (usually HDU) for 24 hours observation.
Airway, breathing
Some craniofacial patients may have a difficult airway either secondary to an underlying syndrome and/or secondary to hardware placed at surgery.
a) Identify any potential risk factors with anaesthetics at handover.
b) If headgear is in place: make a contingency plan with anaesthesia and surgeons for the rare occasion when an emergency re- intubation is required. Ensure appropriate equipment is at the bedside in order to facilitate this.
Cardiovascular
Craniofacial surgery can be associated with substantial blood loss particularly in young children.
All children will return with an arterial line in-situ.
The majority of patients will return with a sub-galeal (scalp) drain in-situ (see image) and pressure bandage. If bleeding from pressure dressing contact Cons. Surgeon.
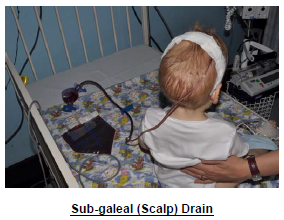
The drain must never be re-vacced. Occasionally the drain will not be vacced at surgeon discretion. If bandage falls off - replace
Monitor closely for signs of continuing blood loss: High drain losses, tachycardia, cool peripheries, poor U/O. A urinary catheter should be in-situ.
- For the initial 3-4 hours drain losses should be replaced with the same volume of packed red
cells (if minimal blood loss use clinical discretion):
The drainage system is less accurate than those used for cardiac patients – the drain losses
only need to be approximate. It is very obvious if a patient is bleeding a lot.
- Initial drain losses are usually about 3-5ml/kg/hr
- If drain losses are higher than this inform the Consultant surgeon
- Hb should be kept above 70g/l (Hb almost always falls post-op)
- After this time, further management depends on the amount of drain loss:
- If drain losses are minimal (<1 ml/kg/hr) and Hb acceptable then losses no longer need to be replaced
- If drain losses are still high or if Hb is low then further blood replacement is required.
FBC and a repeat coagulation screen should be sent in this situation as occasionally clotting factors are required. The Consultant surgeon should be informed.
Tachycardia –Common. Consider if secondary to pain, blood loss, pyrexia, too tight bandage, blocked catheter etc. Some patients remain tachycardic for 24 hours
Neurology
Patients should be nursed at 45o.
Neurological examination documented and neurobservations commenced.
An uncommon but important complication of surgery is clot formation (scalp /extra-dural/subdural). Therefore need to be vigilant with neuro-obs. Important changes are rarely subtle.
Neurobs:
- Every 30 mins for the first 4 hours.
- Every hour for the next 4 hours.
- Then 2 hourly
It is particularly important to assess and document pupil reaction. Craniofacial cases inevitably develop marked diffuse bruising and swelling of eyes in the first 24 hours which subsequently makes pupil assessment impossible.
Any changes in neurology should be taken seriously. The Consultant neurosurgeon should be informed and CT scan arranged.
Monitor for any evidence of CSF leak (nose). Contact Cons. Surgeon.
Pain management
Patients usually arrive with a standard morphine NCA/PCA for first 24 hours.
Regular paracetamol is prescribed. Ibuprofen can be added in addition.
Fluids
0.9% saline is standard IV fluid (+/- dextrose) – 70% restricted
Patients are encouraged to eat and drink as usual as soon as they feel able to.
Antibiotics
Flucloxacillin 25mg/kg is prescribed for a further 2 doses post-op.
(Teicoplanin 10mg/kg if allergic)
Steroids
At surgical discretion- see operation note.
Bloods
FBC, U&E, coagulation screen and gas is performed on admission.
Vomiting
PRN ondansetron prescribed. However remember vomiting can be associated with raised ICP.
Pyrexia
It is not unusual to develop a pyrexia in the first 24 hours. First step should be to remove tight head bandage. Re-bandage with light dressing, then consider other causes.
- Morning bloods: FBC, U&E, coagulation screen and gas.
- TPR and Neuro obs (4hourly for 48hours)
- Remove arterial line and urinary catheter if stable.
- Following neurosurgical/maxillofacial review – discharge to ward.
Drains often stay for 48hours. At surgical discretion drain may be removed. - Morphine PCA/NCA can usually be discontinued. Alternate regular paracetamol and ibuprofen should be prescribed. Oramorph prn.
- Mobilise
- Patient will be discharged to surgical ward – General surgery registrar to be
informed and ward doctor. - Ensure post-op management nursing plan paperwork sent with discharge.
Last reviewed: 03 November 2015
Next review: 30 November 2020
Author(s): Anne McGettrick
Approved By: Clinical Effectiveness
Reviewer Name(s): Paediatric Clinical Effectiveness & Risk Committee

