Large bore veno-venous lines (e.g. "GamCaths") - SOP for first usage and troubleshooting
exp date isn't null, but text field is
Objectives
For lines used in extracorporeal renal and/or haematological therapies such as CVVD, IHD, Plasmapheresis or Plasmafiltration.
- To allow standardised verification of correct placement of venovenous haemodialysis/filtration lines in the Paediatric PICU.
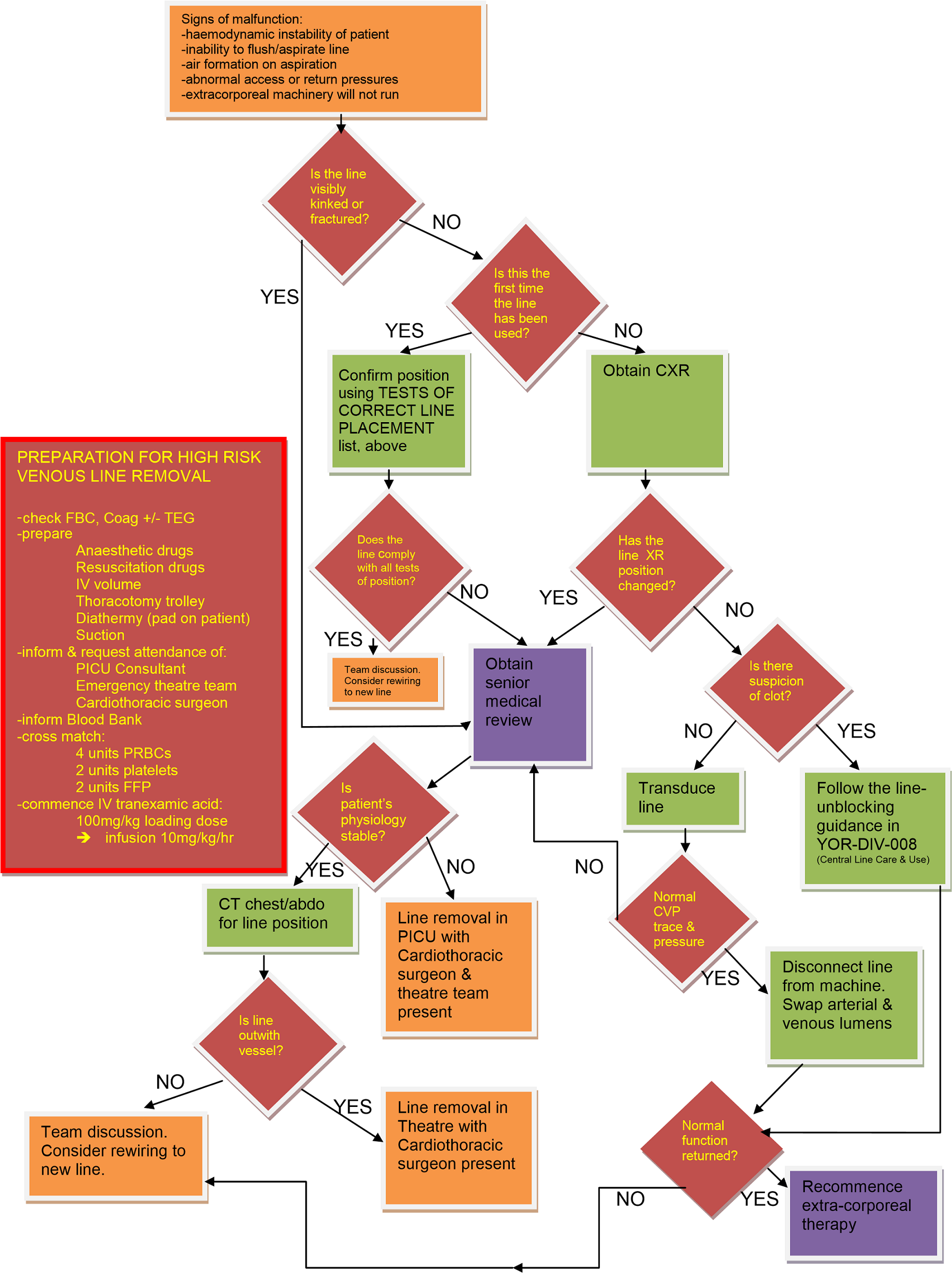
- To provide an evidence base and a clear procedure for the management of a suspected misplaced or blocked line.
- To provide educational material to assist staff managing a child with such a line in the PICU.
Scope
- This SOP applies to the immediate first use and subsequent troubleshooting of veno-venous haemodialysis/filtration lines in PICU.
- This SOP is intended to complement the hospital guidance given in the NHSGGC Vascular Access Procedure and Practice guideline, and also the RHC Renal Unit guidance in YOR-REN-001, but with specific reference to devices used for extracorporeal renal and or/haematological therapies in PICU.
Audience
Standard Operating Procedure for the Paediatric Intensive Care Unit (Ward 1D) Royal Hospital for Children, Glasgow.
All healthcare professionals involved in caring for patients with such lines in the PICU should be aware of this Standard Operating Procedure.
These lines are large diameter (8Fr – 12Fr), stiff plastic central lines with 2-3 lumens. Unlike standard central venous lines, they are relatively rigid to enable them to cope with the negative pressures generated by extracorporeal circuits. They come in temporary (non-tunnelled) and longer-term (tunnelled) versions. Most children in PICU will have had a temporary line inserted at the bedside by a member of PICU staff. Patients who are stable enough and who are going to need longer term treatment, may have a tunnelled line inserted in theatre.
Both types of lines can be connected to various different types of extracorporeal circuits to enable a range of extracorporeal treatments including Continuous Veno-venous Haemofiltration (CVVH), Intermittent Haemodialysis (IHD), Plasma Exchange, Plasmapheresis and Plasmafiltration.
Haemorrhage
Because of their large bore and relative inflexibility, these lines have greater potential to cause blood vessel damage and bleeding than a standard central line. Haemorrhage can occur due to vessel tears at the time of insertion, or due to traumatic erosion of the vessel wall during use. Adult case series give a haemorrhage risk of approximately 2.5-3% per 100 line days from this type of line.
Clot
These lines can completely occlude the great veins in smaller patients, leading to venous stasis, congestion and risk of venous thrombosis. The lines themselves can also become obstructed with clot, particularly during periods of non-use, or conditions of marginal flow or under-anticoagulation. Care should be taken to HepLock the lines when not in use (see separate document: YOR-REN-001) and to ensure good blood flow and adequate anticoagulation during use.
Deep venous thrombosis is also a major risk during interruptions in extracorporeal therapy. For patients who are under 5kg in weight, or who are in a prothrombotic state, or who have a vessel diameter <5mm, serious consideration should be given to continuing systemic anticoagulation during breaks in therapy while the line remains in situ.
Misplacement
Our institutional experience shows that even highly experienced operators can misplace these lines during the insertion process. This is a particular risk with internal jugular placement, where lines can penetrate the carotid artery, the dome of the pleura, the right atrial wall or the deeper mediastinal tissues.
Migration/Displacement
After placement, lines can migrate & become displaced, particularly in mobile patients. Non-tunnelled lines are particularly susceptible to displacement due to changes in patient position or superficial tissue oedema causing the line to pull back. Lines can also erode the wall of the great veins or the right atrium, causing haemorrhage and/or tamponade.
Kinking/fracture
These lines are designed to be quite rigid in order to withstand negative hydrostatic pressures. This rigidity gives the line plastic a ‘memory’ and makes them prone to kinking. This is a particular risk for mobile patients with a line in the femoral position, where repeated flexing of the hip joint will cause kinking over time. Kinked lines can fracture, causing haemorrhage, bloodstream infection risk and/or air embolism. They should therefore be exchanged for a new line as soon as significant kinking is discovered. Consideration should be given to a tunnelled upper body line in such cases.
Infection
All central venous lines present a risk for Central Line-Associated Bloodstream Infection (CLABSI). Insertion should follow the infection prevention procedures laid down in the central venous access checklist. During subsequent use and routine maintenance, standard handwashing and central venous access hygiene procedures must be followed to reduce this risk. The line should be removed at the earliest possible opportunity after it is no longer needed.
Before first use of a new line for extracorporeal therapy, care should be taken to confirm that the line is definitely in the intended correct blood vessel. All four of the following techniques should be used to confirm that the line is in a vein:
TESTS OF CORRECT LINE PLACEMENT
- Direct SonoSite ultrasound visualization of the vessel in both transverse & longitudinal planes following insertion
- Confirmation that both lumens of the line can be aspirated and flushed with minimal resistance.
- Pressure transduction of main lumen shows a CVP waveform and a mean pressure appropriate to that patient’s expected CVP.
- For internal jugular lines, chest X-ray confirmation should show the line following the expected path of the internal jugular vein. The line tip should be outside of the cardiac silhouette.
Last reviewed: 17 August 2021
Next review: 01 September 2024
Author(s): C Begg, N Spenceley, K McCool, J Grady
Version: 1.3
Approved By: PICU Guidelines Group