Temperature management : axilla temperature (Tempa.DOT) (PCCU)
exp date isn't null, but text field is
Objectives
Temperature measurement is a commonly used assessment parameter when caring for acutely and critically ill children. In the critically ill child an abnormal temperature may reflect changes in their physiological status. Therefore, temperature measurement and temperature trends must be accurate and consistent, as decisions about therapeutic intervention may be based upon it.
Pulmonary artery temperature measurement was considered to be the ‘gold standard’ for measuring core body temperature. However, in practice this is too invasive and not a practical method of thermometry. Instead, body temperature is usually measured from a site, or ‘shell’ sites that are thought to reflect the core temperature. The site and measuring device chosen is based upon a number of factors including age, clinical condition, degree of accuracy required, safety and ease of use. It is responsibility of the nurse to determine the best method for monitoring patient temperature and to use the temperature monitoring device correctly. Whichever site/equipment chosen, the nurse must be aware of the benefits and limitations of each.
This nursing procedural guideline is intended as a resource for nursing staff involved in caring for children in the Paediatric Critical Care Unit that require monitoring and measurement of body temperature. The guideline has been constructed after literature search and review of sourced textbooks, Medline and CINAHL, and external nurse expert peer review and opinion.
See also recommendations and further information at end of this guideline.
Scope
This nursing procedural guideline is intended to be followed by nurses involved in caring for the highly dependent or critically ill infant or child requiring body temperature monitoring within the Paediatric Critical Care Unit at the Royal Hospital for Children, Glasgow.
Audience
All nursing staff involved in the measuring and monitoring of temperature in the Paediatric Critical Care unit should be familiar with this nursing procedural guideline.
|
 |
|
PROCEDURE: |
RATIONALE |
|||
|
Provide age appropriate explanation of procedure |
To ensure the child (and parent) understand and consent to the procedure. |
|||
|
Wash hands thoroughly with appropriate skin cleanser. |
To minimise the risk of cross infection. |
|||
|
Choose temperature measurement device (E.g. Tempa•DOTTM) and document which type chosen. Where possible use same type of equipment and site each time. |
To ensure consistency in temperature readings. Switching between sites and changing from one type of thermometer to another can produce misleading results |
|||
|
For Tempa•DOTTM: Ensure Tempa•DOTTM packaging is sealed prior to use and does not appear opened. Check expiry date on packaging prior to use. |
To ensure that ambient temperatures do not interfere with the chemical dots and influence the reading. To ensure the Tempa•DOTTM has not been exposed to ambient air and is clean, unused and suitable for use. |
|||
|
Lift the infant or child’s arm and place the Tempa•DOTTM in the axilla apex, halfway between the anterior and posterior margins of the axilla with the dot matrix against the torso.
Then ensure the arm is ‘held’ or placed in a position that keeps the Tempa•DOTTM thermometer between the two skin folds. |
This position is thought to be the warmest point in the axilla.
To ensure a more accurate reading by not exposing the thermometer (and the chemical dots on it) to the air. |
|||
|
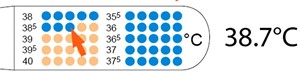
Keep the Tempa•DOTTM in situ for 3 minutes - then it can be removed.
Once removed the nurse should wait a further 10 seconds. The nurse should then look at the Tempa•DOTTM and check that the dots have changed in colour from beige to blue, with the last blue dot indicating the infant or child’s temperature. The nurse should now read and document the infant or child’s temperature and site taken from. E.g. axilla. |
To ensure the chemical indicator dots have time to change and measure the infant or child’s temperature. The accuracy of the reading will be affected if the Tempa•DOTTM is not kept in for the recommended time.
Once the Tempa•DOTTM is removed from the infant or child, a stabilization period of 10 seconds is required to ensure the temperature reading is constant. |
|||
The axilla site for temperature measurement is thought to be a convenient, safe and accessible route of non-invasive temperature measurement. There is a reduced risk of physical or psychological trauma when using the axilla, and this route can be used from infancy to adolescence. Although it is not a core site, some authors suggest that core temperature can be estimated reasonably accurately using the axilla route and that it can provide useful information on temperature trends.
However, the accuracy of the axillary site is affected by a number of factors including ambient temperature, local blood flow, inappropriate placement and temperature differences between left and right axilla. Furthermore, when taking an axilla temperature, the nurse must be aware of the recommended placement times for each type of thermometer, as not keeping the thermometer in place for too short or for too long a period, can affect the temperature reading adversely.
Some studies show that axilla temperature measurements can sometimes appear to be lower than the ‘Gold standard’ pulmonary artery temperature and that even with correct positioning, is much slower in registering changes in core temperature. As such, the nurse must be aware that during extreme thermal perturbations accuracy is significantly reduced.
If the nurse finds any abnormal temperature measurements using axilla technique then the nurse must recheck the temperature and also consider another method & site of thermometry. Any abnormality must be documented and reported to nurse-incharge and doctor.
- Amoore, DA (2010) Best practice in the measurement of body temperature. Nursing Standard, Vol. 24 (42), pp. 42-49.
- Bailey, J Rose, P (2001) Axillary and tympanic membrane temperature recording in the preterm neonate: a comparative study. Journal of Advanced Nursing, Vol. 34 (4), pp 465-474.
- Charafeddine, L Tamim, H Hassouna, H Akel, R Nabulsi, M (2014) Axillary and rectal thermometry in the newborn: do they agree? BMC Research Notes, Vol. 7, No. 584.
- Cincinatti Children’s Hospital Medical Center (2011) Axillary Temperature Taking Tools: The Evidence for Change. Cincinatti Children’s Hospital Medical Center: Cincinatti OH.
- Dougherty, L, Lister, S (2015) Observations: Temperature. In: The Royal Marsden Hospital Manual of Clinical Nursing Procedures. (9th Ed). Blackwell Publishing, London.
- Farnell, S Maxwell, L Tan, S Rhodes, A Philips, B (2005) Temperature measurement: comparison of non-invasive methods used in adult critical care. Journal of Clinical Nursing, Vol. 14 (5), pp 632-639
- Hutton, S Probst, E Kenyon, C Morse, D Friedman, B Arnold, K Helsley, L (2009) Accuracy of different temperature devices in the post partum population. Journal of Obsterics, Gynacology and Neonatal Nursing, Vol. 38 (1), pp 42-47.
- Jackson Barton, SJ Gaffney, R Chase, T Rayens, MK Piyabanditkul, L (2003) Pediatric temperature measurement and child/parent/nurse preference using three temperature measurement instruments. Journal of Pediatric Nursing, Vol. 18 (5), pp 314-320.
- Klein, M DeWitt TG (2010) Reliability of parent-measures axillary temperatures. Clinical Pediatrics, Vol. 49 (3), pp. 271-273.
- Martin, S Kline, A (2004) Can there be a standard for temperature measurement in the pediatric intensive care unit? Advanced Practice in Acute Critical Care: Clinical Issues, Vol. 15 (2), pp 254-266.
- McQueen S (2001) Clinical benefits of 3M TempaDOT thermometer in paediatric settings. British Journal of Nursing, Vol. 10 (1), pp 55-58.
- Medical Indicators (2014) Tempa DOT TM technical information and Tempa DOT TM axillary thermometer
- Molten, A Blacktop, J Hall, CM (2001) Temperature taking in children. Journal of Child Health Care, Vol. 5 91), pp 5-10.
- Moran, DS Mendal, L (2002) Core temperature measurement: Methods and current insights. Sports Medicine, Vol. 32 (14), pp 879-885.
- NICE (2007) Clinical guideline 47: Feverish Illness in children. Assessment and initial management in children younger than 5 years. NHS, London.
- Otto, MA (2017) Axillary thermometry is best choice for newborns. The Hospitalist.
- Sessler DI (2008) Temperature monitoring and perioperative thermoregulation. Anesthesiology, Vol. 109 (2), pp 318-338.
- Sund-Levander, M Grodzinsky, E Loyd, D Wahren, LK (2004) Errors in body temperature assessment related to individual variation, measuring technique and equipment. International Journal of Nursing Practice, Vol. 10 (5), pp 216-223.
- Sund-Levander, M Grodzinsky, E (2010) What is the evidence base for the assessment and evaluation of body temperature? Nursing Times, Vol. 106 (1), pp. 10-13.
- Van den Bruel, A Aertgeerts, B De Boeck, C Buntinx, F (2005) Measuring the body temperature: How accurate is the Tempa Dot®? Technology and Health Care, Vol. 13 92), pp. 97-106
- Wilshaw, R Beckstrand, R Waid, D Schaalje, GB (1999) A comparison of the use of tympanic, axillary and rectal thermometers in infants. Journal of Pediatric Nursing, Vol. 14 (2), pp 88-93.
Last reviewed: 09 May 2022
Next review: 09 May 2025
Author(s): Jeanette Grady
Approved By: PICU Guideline Group
Reviewer Name(s): L. Moore