Paediatric Early Warning Score: PEWS
exp date isn't null, but text field is
Objectives
The purpose of this document is to provide guidance for nurses and clinicians on using the standardised PEWS chart and may be used in conjunction with the National Paediatric Early Warning Score Chart Training Package.
The PEWS charts are available on the Scottish Patient Safety Programme site.
Scope
The contents of the guidance applies to all practitioners employed by, or working on behalf of NHS Greater Glasgow and Clyde (NHSGGC), on a substantive or temporary basis who are undertaking observations on children within NHSGGC.
Vital signs and observations are essential to assess the child’s clinical status; using Paediatric Early Warning Score (PEWS) system enables the early recognition of sick patients and management of any deterioration.
Vital signs include heart rate, respiratory rate, blood pressure, oxygen saturation and temperature.
Observations require your clinical judgement and include assessing levels of consciousness, capillary refill time and acting on staff and/or carers concerns.
For purpose of this document the term ‘observations’ includes both vital signs and observations; and ‘child’ and or ‘children’ refers to any infant, child or young person undergoing care within NHSGGC.
The National Paediatric Early Warning Score (PEWS) was introduced to improve communication of the deteriorating child from one health board to another. Previously there had been 14 different early warning scoring charts, all scoring differently. Maternity and Children’s Quality Improvement Collaborative (MCQIC) agreed on the standardisation of an early warning scoring system to be used across Scotland. There are five age appropriate charts (0-11mths; 12-23mths; 2-4yrs; 5-11yrs ;> 12years).
Observations recorded on the Paediatric Early Warning Score (PEWS) include respiratory rate, heart rate, blood pressure, oxygen saturation, temperature, level of consciousness and capillary refill time. A non physiological parameter which is scored is oxygen therapy.
Staff and /or carers concerns are also recorded and should overrule the necessity of a certain score to escalate concerns.
Regular recording and assessment of observations are used to detect any signs of serious illness or deterioration and provide the necessary information of how a child’s illness is responding to treatment.
Combining and monitoring observations over time creates situation awareness of a child’s clinical status that can be shared with other team members.
In addition, using triggers from one parameter, for example; raised heart rate, should promote information seeking from other parameters, e.g. blood pressure and capillary refill time as they both will enhance the clinical picture.
Therefore, if observations trigger an increase in the PEWS score above 0 or there is concern about the patient’s condition, the clinician should assess and measure all parameters to enhance the clinical picture.
Assessment and documentation of observations should continue to be undertaken at a prescribed frequency as clinically appropriate to the child’s needs.
Clinical acumen and judgement remain essential for the detection of deterioration in a child with mild or no abnormal physiological observations.
Clinical observations that should be carried out at the prescribed frequency include:
- Heart rate
- Respiratory rate
- Peripheral oxygen saturation (SpO₂)
- Temperature
- Level of consciousness using the alert, voice, pain, unresponsive (AVPU) scale; please note if patient is asleep
- Blood pressure
- Capillary return time
- Oxygen therapy
Where there are concerns of serious illness and deterioration, or for those children undergoing high risk treatments; for example, chemotherapy, blood transfusion, or for a specific disease pathway, more frequent checks of observations may be required.
A complete set of observations including blood pressure is undertaken on ALL children:
- Within one hour of admission to the ward / department, thereafter serially recorded at a prescribed frequency dependant on the child’s clinical condition
- Where there are concerns of serious illness and deterioration.
- During an acute phase of the child’s hospital admission, a minimum of four hourly observations and more frequently as condition dictates.
- Post-operatively, frequency of observations should reflect the child’s clinical condition or risk of deterioration (RCN, 2017).
- During and after receiving a blood transfusion as per guideline (Blood Component Prescription & Record of Transfusion Document, NHSGGC).
- Chemotherapy or other high risk treatments.
- With a decreased level of consciousness (in addition, Paediatric Neurological observations rather than AVPU should be assessed).
- With an increase in PEWS score.
- Staff and/or carer concern.
Each set of observations taken must be scored using PEWS and the appropriate action taken as set out in the escalation guide on the PEWS chart.
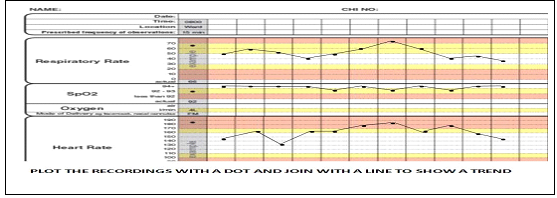
The PEWS chart and score is specifically designed to enhance the identification of changing trends in observations. It is important to watch for declining or no improvement in trends and escalate concerns to the appropriate staff.
Trends are more easily seen if the ‘dots’ on the chart are connected by straight lines.
Recording of observations may be performed by health care support workers, assistant practitioners or nursing students who have received appropriate training; this should be done under the direction and supervision of a registered nurse. These staff must be aware of when they should escalate their concerns.
Abnormal observations recorded by health care support workers, assistant practitioners or nursing students must always be verified by a registered nurse.
When a patient meets the trigger score and the tool is activated, the guidelines regarding frequency of observations and the need for medical assessment should follow the agreed escalation plan.
Parents and guardians can provide information on a child’s normal physiological state; staff caring for them must be aware of this and acknowledge and record any concerns raised.
”Watchers” are children who have clinical indicators which may suggest they are a potential deterioration risk or children for whom there are other clinical concerns, parental concerns, safeguard risk etc. Staff should ensure there is a process in place which allows communication of these concerns to be acknowledged by the clinical teams and locally at the hospital huddles by the Hospital Co-ordinator, which allow discussion of appropriate escalation and plans for identified children and a report/update given to PICU.
Please refer to the ‘watcher criteria’ located in clinical areas (appendix 1).
Some children will transgress the PEWS criteria in their normal state due to chronic illness; where this occurs medical and nursing staff must jointly agree and set alternative parameters to ensure that they can be alerted to potential deterioration.
The PEWS tool does not replace clinical judgment. If a child is deteriorating acutely or is in peri-arrest call the resuscitation team on 2222.
REMEMBER: If the child’s observations score 1 or above on the PEWS chart,
- The child they should be reviewed as per the escalation guide,
- A plan of care agreed and documented, which may include investigations or interventions
- Agree when the child is to be re-assessed
Clinical response to a score may vary from the chart escalation guide in areas such as Emergency Department and Theatre Recovery. In these areas, staff should refer to the agreed local escalation guide.
Regardless of PEWS always escalate if you are concerned about a Child’s condition
Concerns include but are not restricted to:
- Gut feeling
- Looks unwell
- Apnoea
- Airway threat
- Increased work of breathing
- Significant increase in oxygen requirement
- Poor perfusion/blue / mottled/ cool peripheries
- Seizures
- Confusion/ irritability/altered behaviour
- Hypoglycaemia
- High pain score despite appropriate analgesia.
You should be aware that a child receiving palliative and end of life care who has triggered PEWS may have a plan in place that may vary the escalation guide. Please refer to any Anticipatory Care Plan (ACP) or Children/Young People Acute Deterioration Management (CYPADM).
See Appendix 2 for further information.
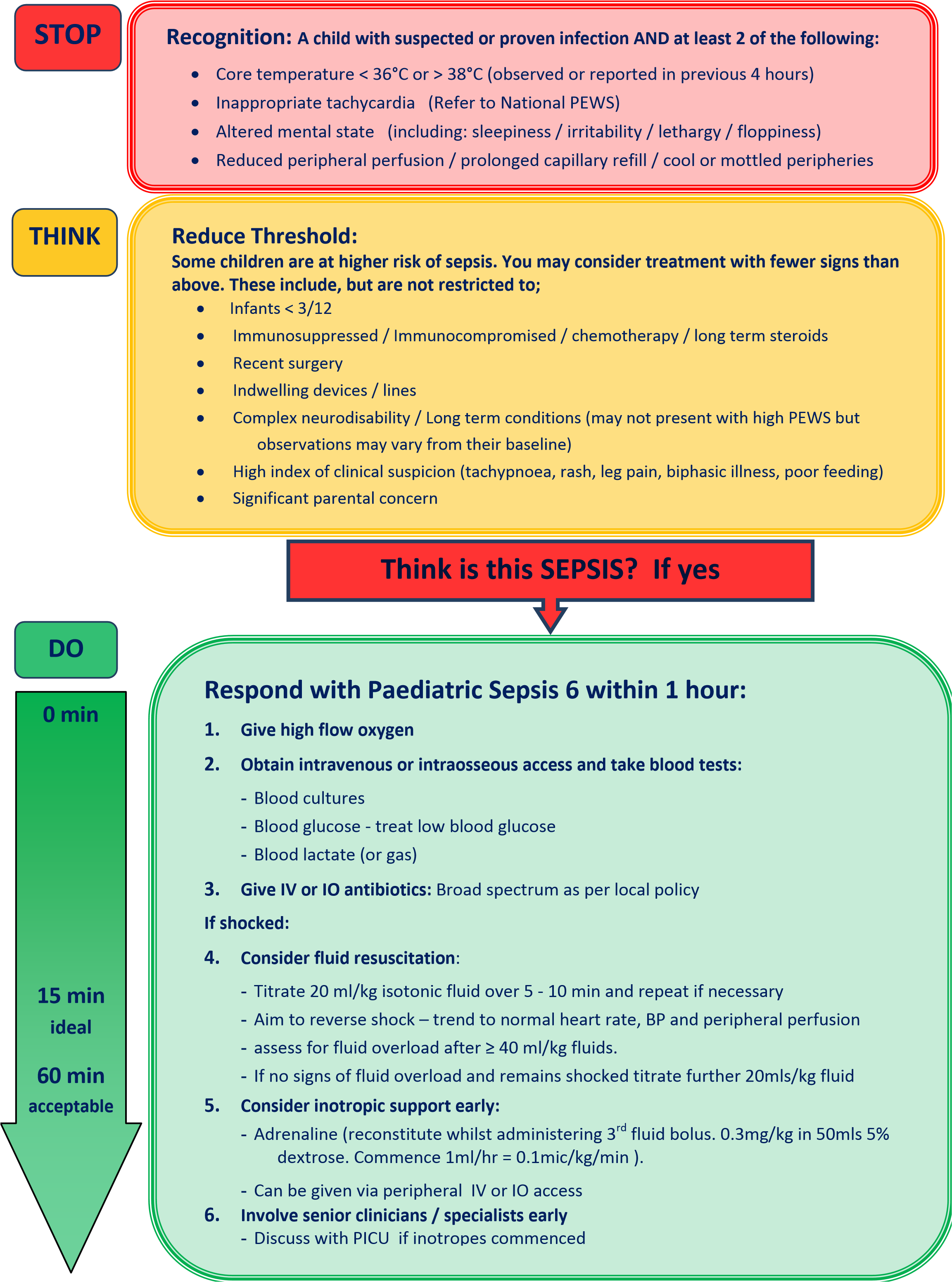
Sepsis is a well known term in healthcare but is poorly understood and under recognised, particularly in children. There are many reasons for this but primarily when it comes to clinical presentation there is a large overlap between infection (normal adaptive response by the body against either an infective agent) and sepsis (maladaptive response by the body against itself which is triggered by infection and is life threatening).
Sepsis should be suspected in any acute illness or in the neonatal population if there are any change from the child’s normal pattern of observations, in particular children with suspected or proven infection.
Sepsis may present initially with non-specific, non-localised symptoms, such as feeling very unwell with normal temperature.
Use your clinical judgement when assessing a child. Not all children with suspected or proven infection has sepsis, however rapid initiation of simple timely treatment following recognition of sepsis is key to improved outcomes.
Sepsis should be considered as a time-critical emergency, as the disease may progress to organ failure, shock, and death very rapidly. Therefore, given the time-critical nature of severe sepsis and septic shock, when sepsis is suspected on clinical grounds, it is usually best to initiate sepsis investigations and treatment and to continue until sepsis has been excluded.
The Sepsis 6 is a set six of interventions which can be delivered by any healthcare professional and must be implemented within the first hour.
The six steps are:
- Give high flow oxygen
- Obtain IV/IO access and take blood
- Give IV or IO antibiotics
- Consider fluid resuscitation
- Involve senior clinicians early
- Consider inotropic support early
(Appendix 3)
Alert/Verbal/Pain/Unresponsive (AVPU) is the simplest assessment tool for level of consciousness for all ages but Neurological Observations may also be required.
If clinically indicated or the conscious level falls to Verbal/Pain/Unresponsive (V/P/U) commence Paediatric Neurological observations. Neurological observations and PEWS should be recorded at the same frequency.
The Paediatric Neurological observations (the Adelaide Coma Scale based on original Glasgow Coma Scale) are an assessment of consciousness looking at arousal, awareness, activity. There are 3 components eye, verbal, motor. It is important to record the best response.
When both PEWS and Neurological observations are recorded on the chart, a new chart must be commenced when either of the scoring tools has used up all available boxes.
(Appendix 4)
- Be vigilant for any indication of pain.
- Pain should be anticipated in neonates and children at all times.
- Children’s self-reporting of their pain is the preferred approach where possible.
- For children who are unable to self-report, an appropriate behavioural or composite tool should be used.
- Assess, record, and re-evaluate pain at regular intervals; the frequency of assessment should be determined according to the individual needs of the child and setting.
- Be aware that language, ethnicity and cultural factors may influence the expression and assessment of pain.
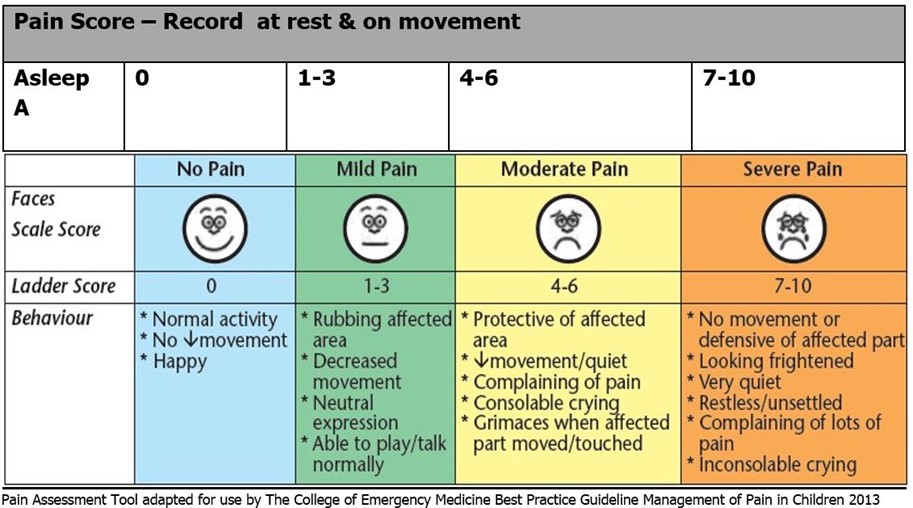
How to score pain
Faces Scale Point to each face using the words to describe the pain intensity. Ask the child to choose a face that best describe their own pain and record the appropriate number.
Ladder Score Discuss 0 being no pain and 10 bring the worst possible pain and record appropriate number.
Behaviour Score:
Awake patient - Observe for 1-5mins or longer; observe legs and body uncovered for tenseness and tone; initiate consoling interventions if needed. Record appropriate pain score.
Asleep patient - Observe for 5mins or longer; observe legs and body uncovered and if possible touch/reposition patient & assess for tenseness and tone. Record appropriate pain score.
A child with a palliative diagnosis may already have an Anticipatory Care Plan (ACP) or a Children/Young People Acute Deterioration Management (CYPADM) form in place. These together or individually provide medical and nursing professionals with guidance regarding how an acute deterioration in a child’s clinical status should be managed. Both documents remain only a guide and have no legal status.
ACP’s are intended to provide professionals with a summary of:
- The child’s palliative diagnosis.
- Past medical history.
- What is important to the child and family?
- Agreed ongoing treatment choices as their condition starts to deteriorate.
- Agreed treatment choices that may no longer be appropriate (IV antibiotics, PICU admission).
- End of life care preferences.
An ACP is agreed and signed by the child’s Lead Clinician and parents and is updated and amended as and when required. ACP’s can be found in Clinical Portal under ‘Care Plans’- ‘Anticipatory Care Plans’. An alert should be created on Trakcare to highlight this.
http://ihub.scot/anticipatory-care-planning-toolkit/
CYPADM’s are intended to provide guidance around the appropriate resuscitative interventions that may be required in management of an acute deterioration. They should not be considered as an equivalent of the adult DNACPR form as a range of resuscitative interventions may be advised including ‘attempt full resuscitation’.
Further information regarding CYPADM can be accessed from:
http://www.gov.scot/Topics/Health/Quality-ImprovementPerformance/peolc/CYPADM
A CYPADM is agreed with parents or young person and signed by their Lead Consultant. Parents have the option to sign but do not need to. A CYPADM holds no legal status and is intended as a guide to what has been previously agreed.
CYPADM’s can be found in Clinical Portal under ‘Legal Notice’- legal notice paediatrics. An alert should be created on Trakcare to highlight this. If a child has a CYPADM in place it is good practice to verbally highlight this at each shift hand over with clear reference made to what resuscitative options have been previously agreed.
Severe sepsis is a CLINICAL EMERGENCY. Early treatment improves outcomes.
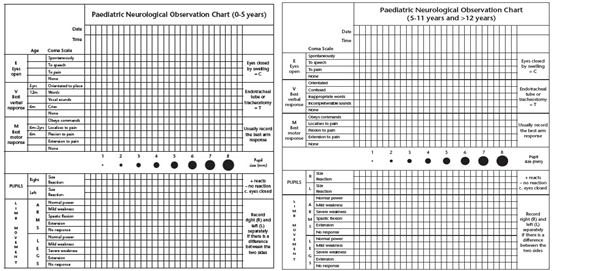
Eye opening:
- If the child doesn't have their eyes open spontaneously as you approach, speak to them in a loud voice or gently shake them; if they open their eyes record this as "eyes open to speech"
- If there is no eye opening to speech, pain is applied by squeezing the trapezius muscle or the ear lobe; if the eyes open record this as "eyes to pain"
- Otherwise the response is "no eye opening"
- If a child has a periorbital haematoma or swelling to the eyes their eye opening response should still be assessed. If it is impossible to open the eyes this is recorded as "no eye opening" and a comment should be made in the nursing chart for the reason why.
Verbal:
- An orientated response is where the child is orientated to time, person and place; they should be aware that they are in hospital, approximately what day or time or day it is and be able to identify family members. A child aged 5 years or older should be able to do this.
- A confused response is when the child does not know the correct answer when asked these questions.
- Inappropriate words occur, when the child makes no attempt to reasonably answer the question, for example just reply yes or no or hiya when asked "Where has Mummy gone"
- Incomprehensible sounds are sounds that are not recognised as words, this includes babbling.
- By six months old, a child should be making incomprehensible sounds (babbling and squeaking etc), by 12 months old they should be saying inappropriate words (mamma or dadda etc).
Motor:
- To see if the child obeys commands, ask them to perform a simple task, for example "stick out your tongue or touch your nose". You can show the patient what you want them to do, particularly important if English is not their first language or they have a hearing impairment.
- If they do not obey, you should test their response to painful stimulation, again by giving their trapezius muscle a squeeze.
- To be recorded as localising, the child must move a hand to the side of the stimulation and above the clavicle.
- If the child flexes the elbow and the wrist, bringing their hand towards their sternum but not above the clavicle, this is normal flexion.
- If the child extends, the arms will remain by their side and the only movement is at the wrist as the hands move outwards.
- Up until 6 months old, a baby will only flex in response to painful stimulation; up until 2 years old they will localise and only when older than 2 years will they consistently obey commands.
Please remember that the best response should be charted; if a child localises with the left upper limb and flexes with the right upper limb, then they are recorded as localising.
Do record what you see, not what you expect to see or what a previous set of observations has been. If you are unsure as a colleague to check.
Barlow,P. (2012) A practical review of the Glasgow Coma Scale and Score, The Surgeon, Journal of the Royal Colleges of Surgeons of Edinburgh and Ireland (10) 114-119.
Clinical Transfusion Policy, NHSGGC [Staffnet link]
Management of pain in children, Best Practice Guideline (2017) Excellence in Emergency Care, The Royal College of Emergency Medicine
National Paediatric Early Warning Score Chart Training Package (2017)
National Paediatric Early Warning Score Charts (2017)
Standards for assessing, measuring and monitoring observations in infants, children and young people (2017) RCN CLINICAL PROFESSIONAL RESOURCE, Second Edition.
The Recognition and Assessment of Acute Pain in Children (2009) RCN.
Last reviewed: 08 October 2020
Next review: 31 October 2023
Author(s): Kathleen Thomson
Version: 2
Co-Author(s): Acknowledgements and Key Contributors to this Clinical guideline: Kathleen Thomson, Senior Nurse Quality Improvement (Main Author); Fiona Clements, Senior Resuscitation Officer; Neil Spenceley, Paediatric Consultant Intensivist; Kay Reilly, Nurse Specialist Pain Management; Emer Campbell, Consultant Neurosurgeon; Lorraine Todd, Neurosurgery Advance Nurse Practitioner; Caroline Porter, Diana Children’s Nurse
Approved By: Paediatric & Neonatal Clinical Risk & Effectiveness Committee
Reviewer Name(s): Dr G Bell; Dr S Young


