Acute replacement of gastrostomy tubes (Emergency Department SOP)
exp date isn't null, but text field is
Audience
For use in RHC Glasgow Emergency Department only
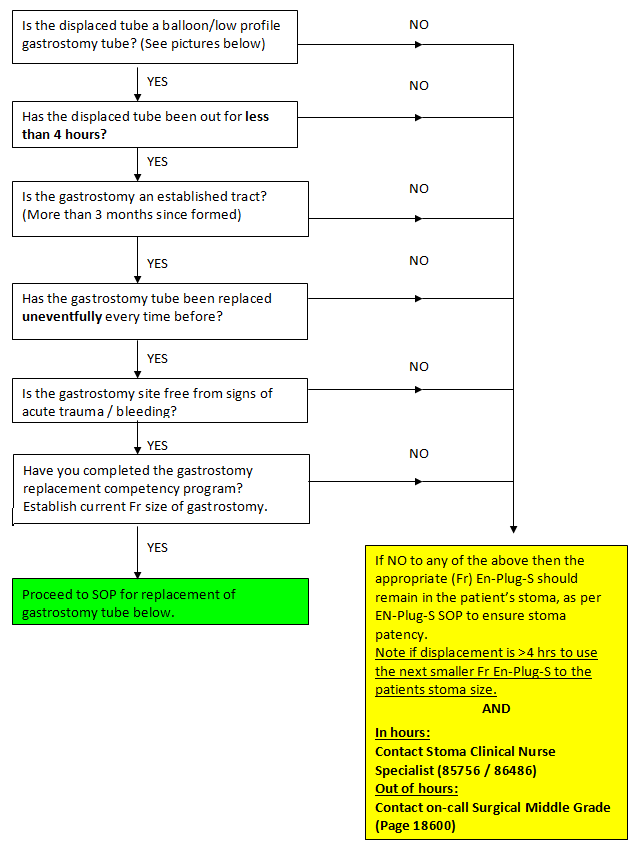
If a patient presents to ED and their Balloon Gastrostomy device has been removed, the following pathway below should be followed.
Initial actions:
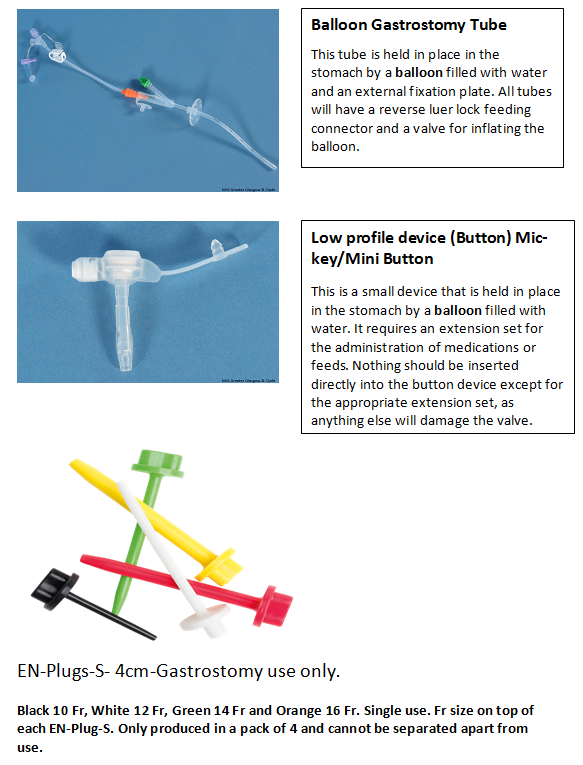
- The Fr (diameter) of the patient’s gastrostomy should be established and length of time the device has been removed, as per SOP below.
- The EN-Plug-S device should then be inserted into the patient’s stoma to ensure stoma patency on arrival to ED by a trained member of the ED team.
- Once the EN-Plug-S device is in situ, the Gastrostomy/Stoma Clinical Nurse Specialist (85756 / 86486 / Nurse Support 85755) should be contacted during working hours (Mon - Fri 8.30am -4pm). Out of hours see below.
If the CNS is unavailable or delayed, the ED Consultant in the department may be able to assist. If not, then the surgical on call registrar should be contacted.
|
SOP for replacement of acutely displaced gastrostomy tubes by ED doctors who have completed the gastrostomy replacement competency program AND in eligible patients only. Stoma patency is priority. If the ED doctor on call has not completed gastrostomy competency program then an EN-Plug-S device must be inserted into the patient’s stoma and CNS or Surgical team then contacted. |
If parent has an appropriate replacement then use this. Check with carer that the balloon G-tube is the correct size (Fr) and length(cm) and in date. If not:
See Gastrostomy trolley in Majors treatment room.
If correct replacement tube not in trolley OR ED Resus store room then contact Theatres for replacement tube or access the store room beside the exit to recovery in surgical day unit.
Confirm which tube should be used – 3 stages:
- Confirm with parents
- Review PORTAL system for details.
- If available look at gastrostomy tube that has become dislodged as the size will likely be on device.
Ask parents which position patient is usually in to have the tube changed. If unsure then position patient supine with abdomen fully exposed.
Discuss analgesia with parent and give if appropriate.
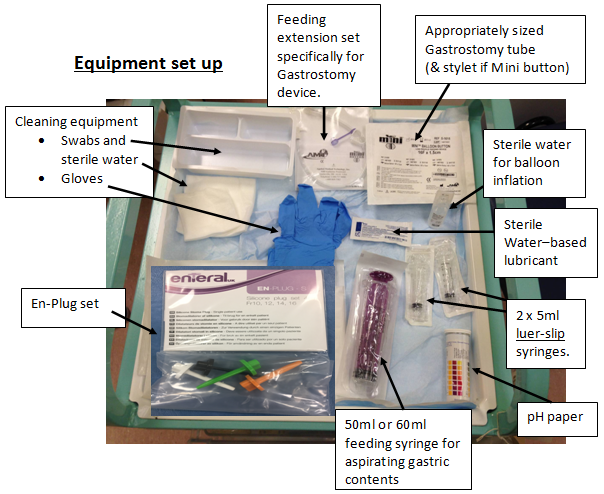
- Area cleaned – use sterile water and gauze
- Balloon check – Use sterile water and ensure balloon inflates easily and dose not leak with volume indicated on device i.e. manufacture advice
(NB for MIC-KEY device use 5mls as standard).
- Mini Button balloon volume stated on balloon valve.
- Appropriate sized replacement gastrostomy tube (calibre and length) available
- ‘Stylet’ for insertion of Mini buttons only.
- Appropriate EN-Plug-S device available (same calibre and smaller sizes) if unable to easily re-site gastrostomy tube as per SOP).
With the balloon deflated, apply a little water-based lubricant to the balloon part of the tube. Insert the lubricated tube into the tract smoothly. It should be a snug fit and a little twist sometimes helps. Excessive resistance should not be encountered. If it is, then insertion may be at the wrong angle. It is possible to make a false passage or insert into the peritoneal cavity. When using a Mini button, push the stylet into the tube until it is 1cm from tip, this should enable easier passage of the button.
Tube position should always be checked after attaching the feeding extension set for the device by attempting to aspirate gastric fluid and testing with pH paper.
PH should be <5.5 – if not then discuss with On-Call Surgical Middle Grade.
NB: In patients on PPI/H2 therapy the pH may not be acidic.
CautionIf there is any doubt about the placement of the tube, contact the On-Call Surgical Middle Grade to discuss whether a contrast study is necessary
If tube placement is confirmed trial with a small, age appropriate, volume of sterile water (i.e. 30mls) to ensure this is tolerated before restarting feeds. Complications with tube replacement likely to arise during or immediately (within 15 minutes) post trial volume.
If there is doubt about position and there is a delay in obtaining confirmatory imaging, patients may require intravenous fluids.
The fluid status of patients MUST be assessed and appropriate fluids given.
If the patient becomes unsettled during recommencing feeds / trial of water, consider the following complications:
- Ileus (this can be identified by the presence of pain associated with reduced bowel sounds and bloating).
- Leakage of feed into the peritoneum (this may be difficult to identify but is typically associated with pain and distress with abdominal distension).
If either of these is suspected, cease feeds immediately and contact the On-Call Surgical Middle Grade for urgent review.
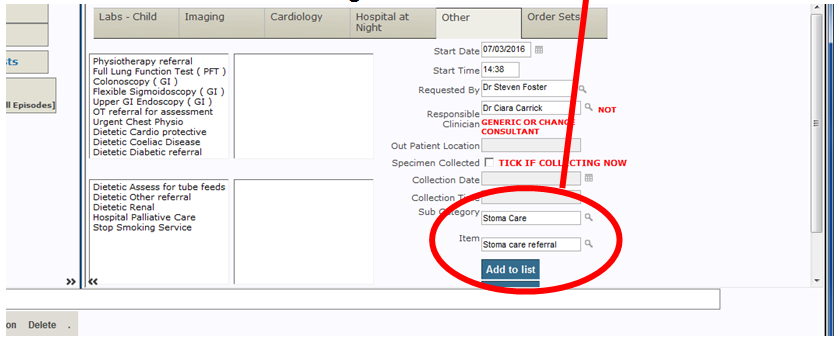
At discharge then please complete TrakCare request as below to inform stoma team of attendance and tube change.
Last reviewed: 09 April 2021
Next review: 09 April 2024
Author(s): Steven Foster
Co-Author(s): Stakeholder: Ms Rania Kronfli (Consultant Paediatric Surgeon, RHCG)
Approved By: Emergency Department

