Hypoglycaemia management, Paediatric Emergency Department
exp date isn't null, but text field is
November 2023: This guidance is currently under review as it has gone beyond the standard review date. It reflects best practice at the time of authorship / last review and remains safe for use. If there are any concerns regarding the content then please consult with senior clinical staff to confirm.
Hypoglycaemia is defined as blood sugar level <2.6mmol/l (commonly referred to as BM). The maintenance of a normal blood sugar level is a complex process.
Hypoglycaemia is a sign of underlying disease that interferes with at least one of the following processes:
- Carbohydrate intake
- Carbohydrate absorption
- Gluconeogenesis
- Glycogenolysis
Gluconeogenesis is a metabolic pathway that results in the generation of glucose from non-carbohydrate substrates e.g pyruvate, lactate, glycerol. It mainly occurs in the liver but also to some extent in the cortex of the kidneys. The process occurs during periods of fasting, starvation, low-carb diets or intense exercise. It is often associated with ketosis.
| Inadequate glucose intake/production? |
OR | Excessive glucose consumption? |
- Starvation
- Malnutrition
- Sepsis
- Malabsorption
- Ketotic hypoglycaemia “accelerated starvation”
- Glycogen storage disease
- Galactosaemia
- Organic acidaemia
- Carnitine deficiency
- Acyl CoA Dehydrogenase deficiency
- Hyperinsulinism
- Hypopituitarism
- Growth hormone deficiency
- Hypothyroidism
- Congenital adrenal hyperplasia
- Hepatitis
- Cirrhosis
- Reye Syndrome
- Aspirin
- Alcohol
- Insulin
- Valproate
The signs and symptoms of hypoglycaemia vary greatly between individuals. Autonomic features tend to appear earlier (but are not always present!). Neurological features occur due to impaired glucose supply to the brain.
| Symptoms | Signs | ||
|
|
Mild
Moderate
Severe |
Sweating
Dizziness |
Tremor Altered consciousness |
- Similar episodes in the past (these may have been unrecognised as being caused by hypoglycaemia e.g seizures)
- Neonatal hypoglycaemia
- Unexplained infant deaths (consider inborn errors of metabolism)
- Some hormone or insulin problems may be familial
Relation to foods
- Milk (galactosaemia)
- Juice (hereditary fructose intolerance)
- Protein (amino acid or organic acid disorder)
- Oral hypoglycaemia agents
- Alcohol
- Aspirin
- B-Blockers
- Insulin
Bloods
Use Paediatric Hypoglycaemia grab bag - Found on all IV trolleys in RHC, Emergency Department.
Details for Paediatric Hypoglycaemia grab bag also found at end of this document.
These bloods are ideally taken before dextrose is given. Aim for 5ml – but minimum 1.5ml.
Bloods should be sent promptly after collection using the POD system. They should be selected as URGENT on Trakcare. It is not necessary to call the lab or sent samples on ice.
Urine
Urinary ketones & Urinary organic acid.
Hypoglycaemia Management Flow Chart
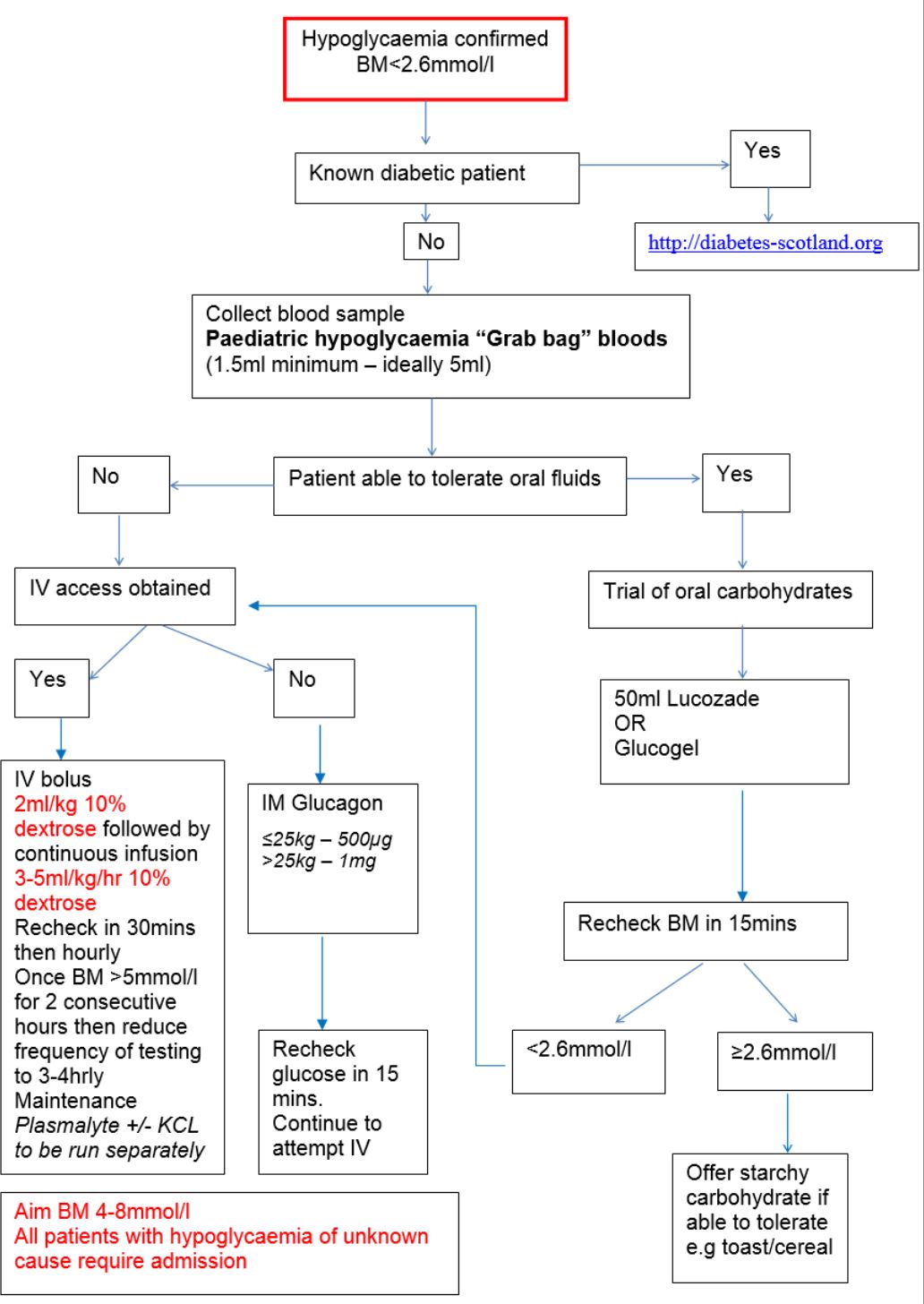
For all patients requiring a 'hypo screen' for hypoglycaemia
|
‘PAEDS HYPOGLYCAEMIA ‐ TIME CRITICAL SAMPLES’
(Samples required PRIOR to administration of glucose)
|
||
| TEST | TUBE TYPE | VOLUME REQUIRED |
| Glucose Free fatty acids (FFAs) |
Fluoride oxalate (GREY) | 500 microlitres (aim for half full) |
| Insulin C-peptide Beta OH butyrate Cortisol |
Lithium Heparin (GREEN screw top) | 1ml ideally 2mls (1 bottle, 2 if possible) |
| Lactate (Capillary blood gas) |
Capillary blood gas tube (Processed in ED) |
Aim for 1 full capillary tube |
***SAMPLES MUST BE IN THE LAB WITHIN 15 MINUTES OF COLLECTION***
CONTACT LAB TO INFORM THEM OF URGENT HYPOGLYCAEMIA SAMPLES
|
'PAEDS HYPOGLYCAEMIA ADDITIONAL ESSENTIAL' |
||
| TEST | TUBE TYPE | VOLUME REQUIRED |
| Ammonia U&Es LFTs CRP Acylcarnitine |
Lithium Heparin (GREEN screw top) | 1ml (1 bottle) |
| FBC | EDTA (Small PINK screw top) | 500 microlitres (up to mark on bottle) |
| Blood culture | Age and volume dependent | |
| URINARY organic acids | URINE in WHITE top universal container | 5mls |
How to order on Trakcare
|
‘PAEDS HYPOGLYCAEMIA ‐ TIME CRITICAL SAMPLES’ |
|
To order the TIME CRITICAL SAMPLES then follow these steps:
**ALWAYS SELECT THE "-CHILD" OPTION FOR THE TEST REQUESTED (WHEN AVAILABLE)** HINTS:
|
|
'PAEDS HYPOGLYCAEMIA ADDITIONAL ESSENTIAL' |
|
To order the ADDITIONAL ESSENTIAL SAMPLES then follow the same process as above. **ALWAYS SELECT THE "-CHILD" OPTION FOR THE TEST REQUESTED (WHEN AVAILABLE)** HINTS:
|
|
ONLY STICK ONE 'TRAKCARE' LABEL TO THE CORRESPONDING TUBE. THE REMAINING LABELS SHOULD REMAIN ON THE REQUEST FORM |
Last reviewed: 29 March 2021
Next review: 30 April 2024
Author(s): Dr Gill Campbell, Paediatric Emergency Department
Co-Author(s): Consulted with: Dr Gufta Shaikh, Paediatric Endocrinology Dept
Approved By: Paediatric Clinical Effectiveness & Risk Committee


