Major Trauma Single Point of Contact (SPOC) SOP – RHCG
exp date isn't null, but text field is
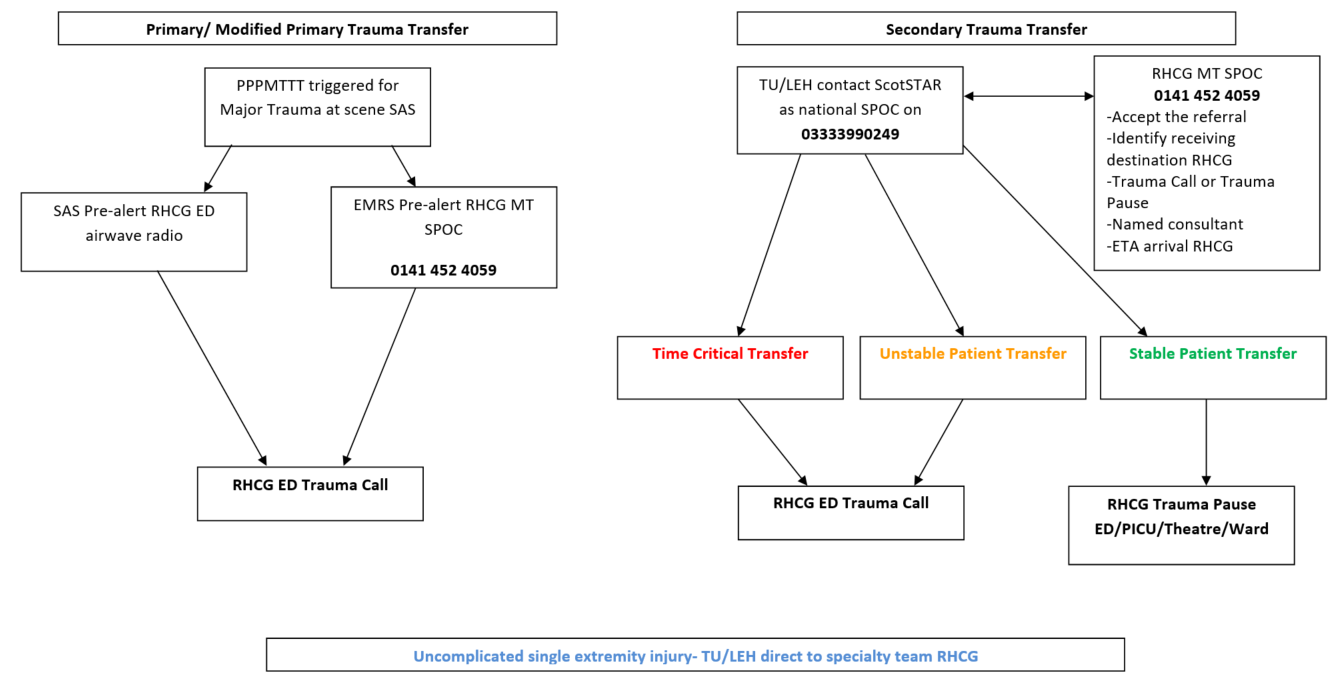
For all secondary/tertiary trauma referrals to Royal Hospital for Children, Glasgow from a Trauma Unit/Local Emergency Hospital, please call 033 33 990 249.
(stable peripheral extremity injuries are generally excluded from this).
For full referral guidance see remaining guideline below.
Objectives:
- To outline the standard operating procedure for the SPOC for RHCG as a Major Trauma Centre (MTC)
- To identify the individual acting as the SPOC
- To outline the roles and responsibilities of the MTC SPOC
Scope:
This document applies to all primary and secondary transfers of trauma patients under the age of 16 to RHCG for MTC level care
Audience:
- Paediatric Emergency Department clinicians and specialty teams with a remit for trauma.
- ScotSTAR retrieval clinicians
- Trauma Unit (TU) and Local Emergency hospital (LEH) clinicians in the WoS with a remit for paediatric trauma
Resources:
This operational plan should be read in conjunction with the following documents:
- STN Paediatric Pre-hospital Major Trauma Triage Tool PPMTTT
- Referral to Paediatric Major Trauma Centres (PMTC) in Scotland: ScotSTAR as the Single Point of Contact (SPoC) Operational Plan
- RHCG Major Trauma Team Emergency Department Activation and Response Standard Operating Procedure
- RHCG Inter Hospital Transfer Policy
ED Majors Consultant: 0141 452 4059 carried 24/7
Between 0800 and 2400 7 days a week this will be carried by a PEM consultant. Out with these times calls will be taken on the same number by a PEM trainee and the on call PEM consultant informed.
(If this number is not immediately answered or busy the ED Co-ordinator number should be used as an alternative 0141 452 4585)
Any child in the WoS that triggers the PPMTTT at scene with SAS or EMRS will come directly to RHCG ED if they are within a 45 minute travel time by road or by air.
SAS will pre-alert RHCG ED as soon as possible via the ED ‘stand by’ airwave radio when the child is en route to RHCG.
EMRS clinicians should contact the RHCG SPOC on the above number to advise that the child is being transported to RHCG and/or for any clinical discussions.
The RHCG Major Trauma Team will be activated by the SPOC to coincide with the patient’s ETA in ED.
Modified primary transfers should be managed in the same way.
For any child that requires transfer from a TU/LEH for MTC level care at RHCG, the referring site will contact ScotSTAR as the national paediatric trauma SPOC as per guidance. The safety of the proposed transfer will remain the remit of the ScotSTAR clinician and not the RHCG SPOC.
The ScotSTAR clinician will bring in the RHCG SPOC, the consultant taking named responsibility (where possible) and any relevant specialty teams to a conference call for initial referral discussions. An automatic acceptance policy applies for these referrals as per the rest of the Scottish Trauma Network.
From these discussions the RHCG SPOC will:
- Accept the referral
- Establish the most appropriate destination for the child on arrival at RHCG
- Establish the most appropriate reception for the child, trauma call or pause
- Establish the clinician taking named responsibility for the patient at RHCG
- Establish the ETA at RHCG or request to be contacted with this once en route
The RHCG SPOC can leave the conference call once the above have been clarified. Clinical support and transfer advice can continue to be provided by the ScotSTAR clinician.
Secondary transfers (including patients that are intubated and ventilated) will fall into the following categories and be managed as follows:
a) Time Critical Transfers
- Will be transferred to RHCG by the referring site to ED at RHCG
- Will have a trauma team response in ED at RHCG
- The RHCG SPOC will assist with the organisation of any imaging and/ or blood products ahead of arrival in conjunction with the responsible team
b) Unstable Transfers
- Will be retrieved by ScotSTAR if non time critical to ED at RHCG
- Will have a trauma team response in ED at RHCG
- The RHCG SPOC will assist with the organisation of any imaging and/ or blood products ahead of arrival in conjunction with the responsible team
c) Stable Transfers (excluding single uncomplicated extremity injuries)*
- Will either be retrieved by ScotSTAR or arrive by paramedic transfer
- Can proceed directly to agreed destination e.g. PICU/ theatre, or be received in ED**
- Will require a trauma pause on arrival at the agreed destination at RHCG
*If the patient is more than 24 hours from admission and coming from an inpatient bed elsewhere for specialist input at RHCG they should be managed as per RHCG’s inter-hospital transfer policy.
** If the patient is to go directly to a destination other than ED in RHCG, the named responsible consultant must be in agreement with this.
d) Stable, uncomplicated single extremity injuries (including fractured femurs)
- Do not require discussion with ScotSTAR as national SPOC or with RHCG SPOC
- Should be a direct specialty to specialty referral
- Should be reviewed on arrival in ED or inpatient bed by the accepting specialty as per the inter-hospital transfer policy**
- A trauma pause can be arranged by the accepting specialty on arrival at the agreed destination at RHCG if deemed appropriate.
|
Primary |
Paediatric patients who are transported to PMTC from scene via Scottish Ambulance Service (SAS) or a pre-hospital medical team. |
|
Modified Primary |
Paediatric patients who are identified on-scene to have injuries likely to require PMTC care however, due to the nature of their injuries, distance or logistical factors, are transferred to a Paediatric Trauma Unit (TU), Local Emergency Hospital (LEH) or community hospital. These patients will have the paediatric retrieval team mobilised before arrival at the receiving unit to assist with initial resuscitation and onward rapid transfer to PMTC. |
|
Secondary |
Paediatric patients who are seen and assessed at TU/LEH but require ongoing care that can only be provided at a PMTC. These patients may be stable, unstable or time-critical. Secondary transfers or interfacility-transfers (IFT) will be classified as per the Intensive Care Society guidelines on transfer of critically ill patients:1
|
|
Tertiary |
Paediatric patients who are assessed at a PMTC but require ongoing specialist care that can only be provided in PMTC in another region. These can be minimised by initially involving ScotSTAR as SPOC, avoiding transfers to a place that cannot provide definitive care. The Intensive Care Society guidelines on interfacility transfers would apply for these patients also. Paediatric patients who have had treatment at a PMTC and require transfer to another PMTC in another region for rehabilitation that is closer to their residence are not considered in this document as they would be classed as repatriations. |
Last reviewed: 07 June 2021
Next review: 07 June 2024
Author(s): Dr Marie Spiers (Joint RHC Clinical Lead for Trauma) & Dr Christina Harry (Joint RHC Clinical Lead for Trauma) on behalf of RHCG