Jehovah's Witness management, paediatric patients
exp date isn't null, but text field is
Objectives
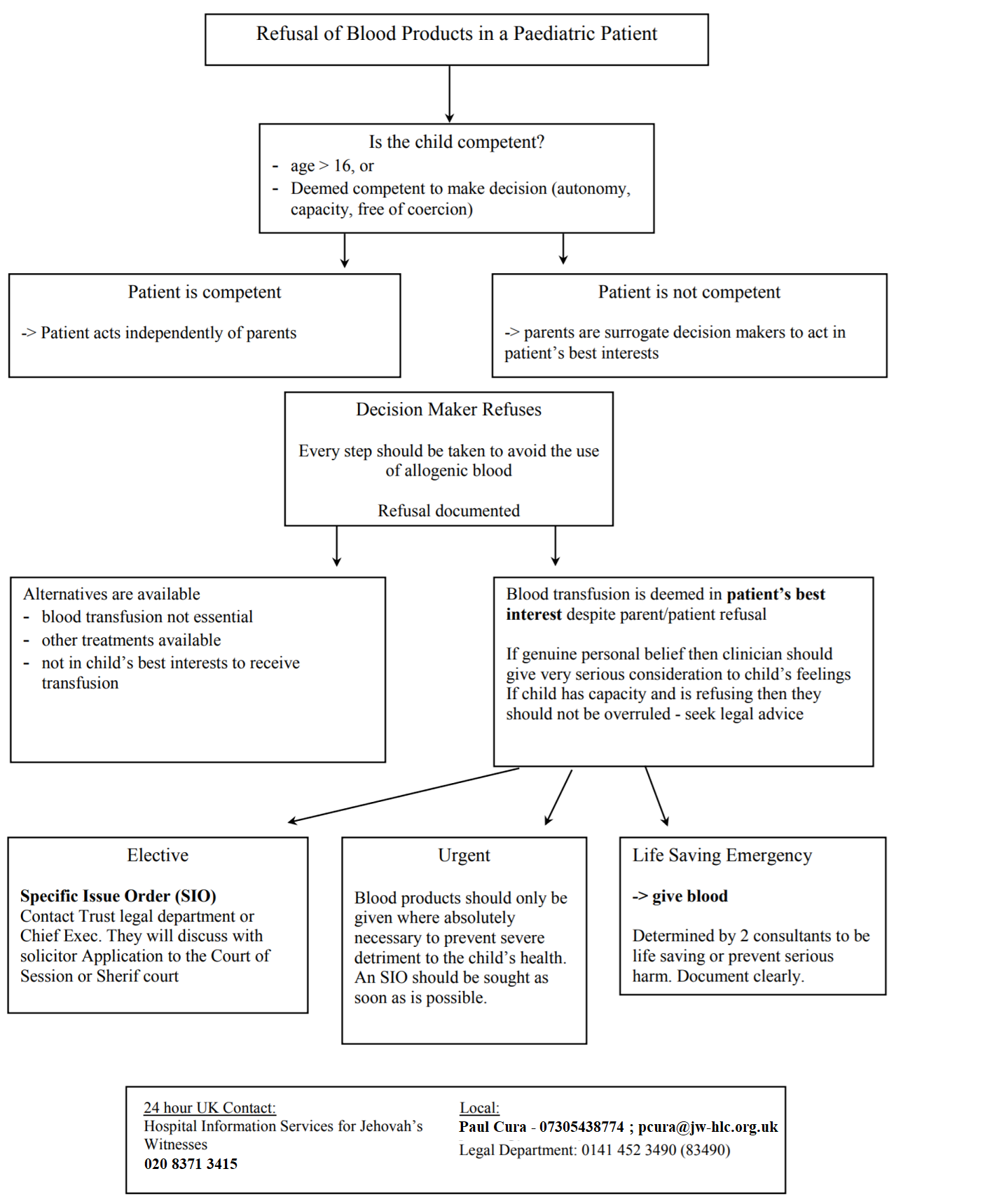
This guideline aims to summarise the considerations of managing a paediatric patient for whom they themselves, or their carer, objects to the use of blood products. It does not aim to provide comprehensive background or discussion. Please refer to existing guidelines including NHS GGC, Association of Anaesthetists, RCS for more detailed information.
Introduction
It is estimated that 140,000 Jehovah’s Witnesses (JW) currently reside in the UK, with 10,000 in Scotland1,2. Jehovah’s Witnesses typically refuse the allogenic transfusion of whole blood and primary blood components. Any non-consensual transfusion would be considered a gross physical violation. Some non-JW patients may also refuse blood and their decision should be similarly respected. The indication for and medical consequence of not receiving blood products should be discussed with each patient and their specific situation.
Jehovah’s Witnesses believe that were a member of their church to ‘wilfully and unrepentantly’ accept a blood transfusion then they will be considered to have left the faith. However, they also report that there is ‘no rejection of those transfused against their will, or in error, or of a child where that action has been taken by clinicians in an effort to preserve health and life’3.
Additional resources available to provide pastoral and liaison support throughout the UK for elective and emergency cases are available at:
|
Hospital Information Desk, 24 hour service: 020 8371 3415 |
Glasgow Local Contacts: Peter Warden - 07974 578897; pwarden@jw-hlc.org.uk Anthony Chali - 07877 312028; achali@jw-hlc.org.uk David Butler - 07722 475834; dbutler@jw-hlc.org |
Capacity
In Scotland, parents cannot give consent at all for young people over the age of 16. If they lack capacity, they should be treated under the guidance laid out in the Adults with Incapacity (Scotland) Act 20003.
A child under the age of 16 can consent to a procedure if they are deemed by a medical practitioner as capable of understanding the nature and consequences of the procedure [Section 2(4) of the Age of Legal Capacity (Scotland) Act 1991]3. As they are considered to have capacity and be competent then they have the right to refuse treatment and neither the parents nor the court can override it in theory, though this has not be definitively tested in the courts3.
Consent
In addition to capacity, consent requires the decision maker to be fully informed of the risks, benefits and alternatives of the treatment, and for this information to be comprehended. In addition, it is essential that the decision is free from coercion.
Ideally, the discussion regarding administration of blood products should be made remote to theatres with adequate time and privacy. As much as it should be clear that a child with capacity has made the decision of their own reasoning and values, it is similarly important that the medical professional also does not aim to impose undue influence on the decision which is not in keeping with the patient’s own wishes and values.
Emergency
In an emergency blood products can be administered in a life-sustaining situation or to prevent lasting disability without patient or parental consent. Two consultants should agree and document the clinical urgency for blood administration2. Legal permission for treatment in the face of parental refusal should be sought at the earliest available opportunity.
Doctor’s Right to Refuse
Should a medical professional feel they cannot work under the proposed constraints associated with refusal to use blood products, a referral to another appropriately skilled clinical or team should be made and recorded in the notes and an appropriate explanation be given to the family3.
Specific Issue Order
A Specific Issue Order, under Section 8 of the Children’s Act 1989, can be made when a child is under 182, with the court acting with the welfare of the child being paramount. The court will make an order, in this situation regarding blood transfusions for the child, superseding parental rights only surrounding this issue. It does not take away any other existing parental rights, and the parents should still be informed of ongoing management plans. Applications should always be made where time permits.
Preoperative
Consent for Blood Components and Procedures
The four primary blood components; red cells, white cells, platelets and FFP are most typically refused. Pre-deposited autologous blood is also generally not acceptable.
The acceptance of primary blood product derivatives is a matter of personal choice. The use of these products should be discussed on an individual basis. Similarly with procedures involving the use of their own blood, including:
- intraoperative or postoperative cell salvage
- Acute normovolaemic haemodilution
- Haemodialysis or haemofiltration - Cardiopulmonary bypass
Optimisation
Schedule early attendance at pre-operative clinics with baseline Hb measurement. Consider EPO/Iron infusions if low Hb. Investigate any clotting or bleeding issues. Withhold anticoagulants and anti-platelet agents where possible.
Multi-disciplinary discussion and planning is imperative.
Intraoperative
All effort should be made to avoid the use of blood products where refused. Consider techniques including:
- Minimise blood sampling
- Maintain normothermia
- Tranexamic acid
- Acute normovolaemic haemodilution if patient suitable
Postoperative
Optimise oxygen consumption and delivery. Repeated blood sampling should only occur when necessary. Monitor post-operative blood loss closely, with early recognition and prompt intervention required.
1. Watson, T., Morrsion, A. “Protocol for Patients who Refuse Blood." NHS Greater Glasgow and Clyde. June 2016.
2. “Caring for patients who refuse blood: A Guide to Good Practice for the Surgical Management of Jehovah’s Witnesses and Other Patients Who Decline Transfusion.” Royal College of Surgeons of England Professional and Clinical Standards. Nov 2016.
3. Klein A., Bailey, C.R. et al. “Anaesthesia and peri-operative care for Jehovah’s Witnesses and patients who refuse blood”. AAGBI Guidelines, 2nd ed. 2005.
Last reviewed: 23 December 2022
Next review: 31 January 2026
Author(s): Ros Lawson, Monique McLeod & Barry Crockett
Version: 2
Approved By: Paediatric & Neonatal Clinical Risk & Effectiveness Committee