MERS - Middle East Respiratory Syndrome - RHC ED patient pathway guidance
exp date isn't null, but text field is
Objectives
MERS-CoV 2018 guidance GG&C
Audience
This guidance is for the use in the RHC ED only.
November 2023: This guidance is currently under review as it has gone beyond the standard review date. It reflects best practice at the time of authorship / last review and remains safe for use. If there are any concerns regarding the content then please consult with senior clinical staff to confirm.
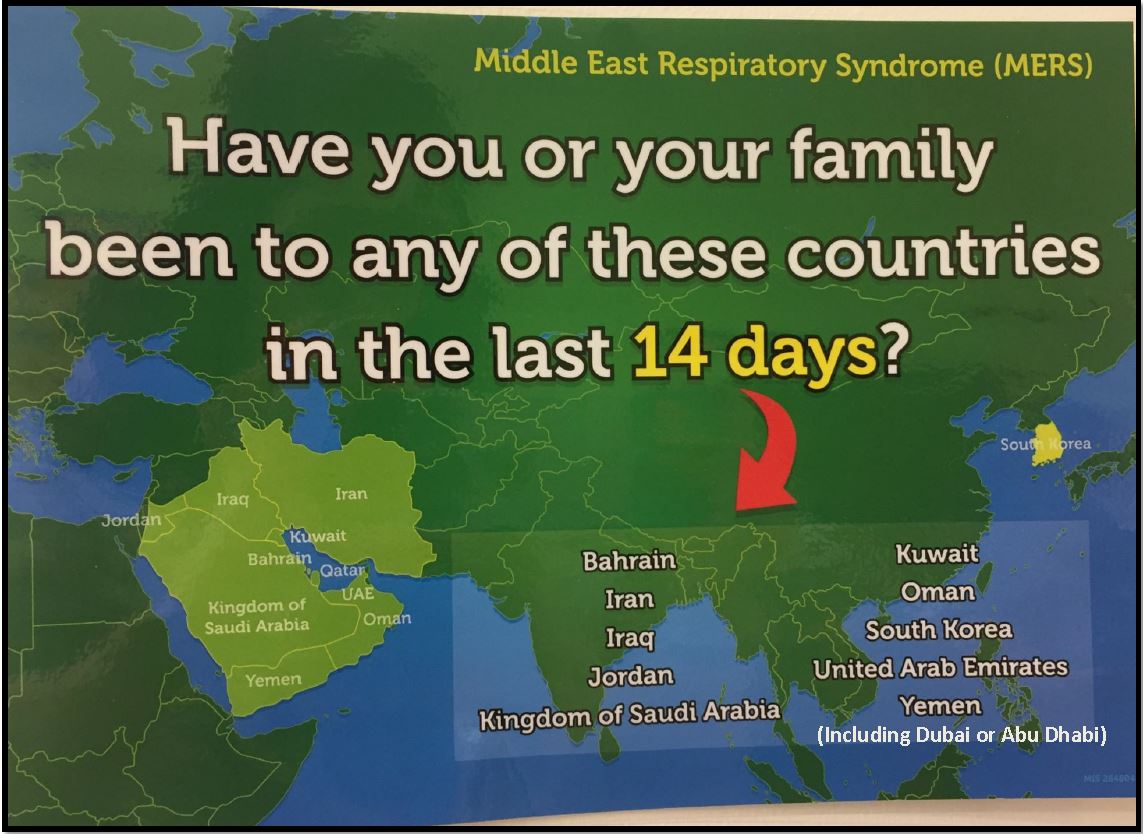
- Reception staff to ask patients if they have been to one of the “MERS POTENTIAL” countries in the last 14 days (see map below).
- MERS potential countries include:
- Bahrain
- Jordan
- Iraq
- Iran
- Kingdom of Saudi Arabia
- Kuwait
- Oman
- Qatar
- United Arab Emirates ((including Abu Dhabi & Dubai)
- Yemen
- South Korea
- If there is a positive travel history to any of the above countries in that time frame, reception staff to ask patient to wait in the breast feeding consultation room across from the reception desk for immediate assessment by the triage nurse.
- Positive travel history –THE PATIENT MUST have been in a “MERS potential” country in the last 14 days before symptom onset and have respiratory symptoms. (NOT patient relative and NOT just transiting through the airport)
- Reception staff to inform triage nurse and ED nurse coordinator immediately.
- Reception staff to take screen shot identifying list of patients in the ED waiting room and in triage queue.
- Breast feeding room to have a terminal clean after it is vacated.
- Triage nurse to wear appropriate PPE (FFP3/Eye protection/gloves/theatre gown) to assess child
- Triage nurse to go to the breast feeding room to confirm that child has respiratory symptoms and give the patient a surgical face mask if possible and take patient/s directly through to room 18 (negative pressure room) in CDU to gather further information.
- If the child is coughing and unable to wear a mask then close all the doors and clear the corridor before moving the child
- Full information gathering should not be done in the breast feeding room or in triage to minimize contamination of rooms and to allow more time to gather the information in a safe and private room.
- If child appears unwell, take the child straight to the resuscitation room.
- Remember lots of children will just have a simple cold. The ones we are concerned about are the ones :
- Unwell enough requiring admission to hospital with severe acute respiratory infection (clinical and/or radiological evidence of pneumonia)
(+) With Fever >/= 38 ⁰c or history of fevers and cough
(+) Together with the travel history
- Unwell enough requiring admission to hospital with severe acute respiratory infection (clinical and/or radiological evidence of pneumonia)
- Patients arriving by ambulance - parents should be asked a brief travel history.
- These potentially unwell MERS patients do NOT go to CDU and are managed in the Resuscitation room.
- Child should be placed at one end of the resuscitation room and the automatic door on that end is sealed with signage restricting access to allow a single point of access.
- Non essential staff are not permitted to access this space.
- Please use resuscitation space 4, if space 4 is being used, please use space 1. If bay 4 is being used, please lock the store room door from the other side to prevent contamination of store room.
- All staff in direct contact with the child MUST wear appropriate PPE.
- All staff in direct contact with the patient must wear appropriate PPE.
- Intubation of a potential MERS child should be done in the Resuscitation room.
- Intubation to be done with a cuffed endotracheal tube and an extra INTERSURGICAL filter should be placed on the patient end. (See picture 1)
- Transfer to PICU- The oxylog ventilator is not a closed circuit so it has been agreed that it should NOT be used for transfer. The child should have an extra INTERSURGICAL filter on the patient end and be bagged up to PICU (See picture 2)
- Transfer – corridor to closest lift. No significant risk to people in corridor unless in close contact with patient.
- Patient should be transfered to Room 5 in PICU
Picture 1.
Picture 2.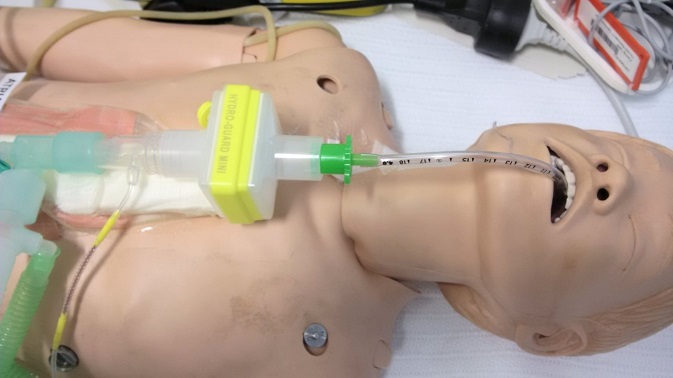
- All non essential medical equipment should be removed from the room before the patient enters
- Initial medical assessment of potential MERS patients should be done by an ED doctor and ED nurse.
- PPE should be worn by the staff at all times.
- Those in PPE should be in communication with a member of staff outside at all times.
- Medical staff to contact Infectious Diseases (ID) and Infection Control (IC) team as soon as possible for advice.
- If the child is unwell, move the child through to the resuscitation room.
- If the child requires admission, the ED doctor will refer the patient to the medical team for further management.
- If the child is well enough to be sent home, virology samples should still be taken (just in case they represent 24 hours later) and the child can be sent home with advice to return if worsening symptoms. This must be done in consultation with the on call Public Health consultant.
- Close each door after patient goes through into room 18 (negative pressure room) in CDU
- Supplies/equipment are available in store room in CDU (right side across from reception desk)
- Move supply/equipment trolley from store room into the negative pressure room (Between the inner and outer door)
- 2 large yellow waste bins are required - One should be placed in the negative pressure room (inside room through both doors) and another between inner and outer doors for contaminated PPE.
- De-robing should take place between inner and outer doors of negative pressure room and contaminated PPE should be placed in the yellow waste bin.
- Medical equipment – should be single use where possible or cleaned as per manufacturers guidelines.
- Where possible attending adults should be restricted in number.
- No attending children should be permitted except in exceptional circumstances.
- Parents of patients should be advised of the risk to them and if well should be given PPE and instructed on how to use it. They can wear an FFP3 mask but will not be fit tested.
- Unwell adult/parent should be assessed for symptoms and remain in CDU pressure room and advised to wear a surgical mask.
- ED doctor to contact Adult ED to discuss management of unwell adult.
- Each department is responsible for their own staff training.
- Training sessions/ refresher sessions on PPE use are run by Tony Brown and Jim Kidd in the ED.
- ED senior charge nurse is responsible for PPE stock in store room in both ED and CDU.
|
CDU Consultant |
84678 |
|
ED Majors Consultant |
84059 |
|
Infection Control Pamela Joannidis (Nurse Consultant and Lead) Angela Johnson (Senior IPCN) Sharon Carlton (Adminstrator) |
80600/ 80326 0141 2011707 0141 4515599 |
|
Infectious Diseases Consultant- Dr Conor Doherty Infectious Diseases Consultant- Dr Rosie Hague Infectious Diseases Consultant- Dr Louisa Pollock |
Page 18418 Page 18078 Mobile via switchboard |
|
Microbiology lab |
89132 |
|
PICU Consultant |
84719 |
|
Resus space 1 |
84042 |
|
Resus space 4 |
84045 |
|
Virology lab (West of Scotland Specialist Virology centre) |
50080 |
Last reviewed: 11 October 2018
Next review: 31 October 2024
Author(s): Steven Foster
Approved By: Emergency Department

